Imaging Pearls ❯ June 2017
|
-- OR -- |
|
Chest
- Lung Cancer Screening
• Can CT be used for the early detection of lung cancer?
• Should CT be used for the early detection of lung cancer?
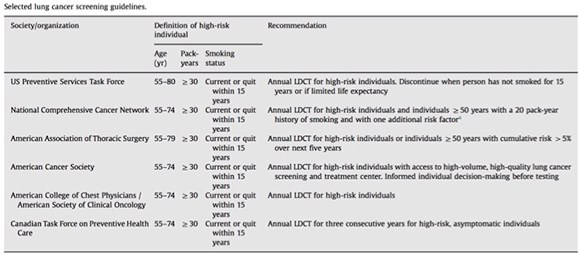
• What is the current status of CT for the early detection of lung cancwr? - Who should be screened?
• Adults aged 55-80 years of age
• 30 pack year history of smoking
• Currently smoke or have quit within the past 15 years
• Exclusions
- Patients who stopped smoking over 15 years ago
- Patient with comorbidities that make the patient a non-surgical candidate - Lung Cancer CT Screening Protocols
• 64 slice MDCT or better
• Low dose scan protocols with 100 kV and 30-100 mA depending on the scanner and availability of iterative reconstruction software
• Slice thickness of 1-1.5 mm slice thickness
• Post processing with MPR (especially coronal) and MIP imagings - Lung Cancer Screening: Challenges
Extra Parenchymal Findings
• Cardiovascular
• Pulmonary (not a nodule)
• Adrenal nodules
• Hepatic lesions
• Renal lesions - “Clinically significant incidental findings on LDCT scans for lung cancer screening are common and their potential impact should be included in the shared decision making process. Screening programs should develop a standard approach for the evaluation of these findings, and consider the financial impact when seeking infrastructure support for screening program implementation.”
The Frequency of Incidental Findings and Subsequent Evaluation in Low-Dose CT Scans for Lung Cancer Screening. Morgan L et al Ann Am Thorac Soc. 2017 Apr 19. doi: 10.1513 (in press) - “The most commonly reported incidental findings were pulmonary (69.6%), cardiovascular (67.5%) and gastrointestinal (25.9%). Fifteen percent of the scans had an incidental finding that resulted in further evaluation. The majority of patients who underwent further testing had cardiovascular findings (10.3%), less frequently thyroid or adrenal nodules (2.1%), hepatic lesions (0.9%), renal mass (0.6%), or pulmonary disease (0.6%). The most frequently ordered investigations were echocardiography (n=9), cardiac stress test (n=9) and CT angiography (n=6). Reimbursement for the screening process, evaluation and treatment of screen detected findings, averaged $817 per screened patient.”
The Frequency of Incidental Findings and Subsequent Evaluation in Low-Dose CT Scans for Lung Cancer Screening. Morgan L et al Ann Am Thorac Soc. 2017 Apr 19. doi: 10.1513 (in press) - “The National Lung Cancer Screening Trial (NLST) is the largest RCT (n=53,454) and compared three annual LDCT scans (the first of which is termed the baseline LDCT) with three annual posterior- anterior CXRs. The NLST trial was conducted at 33 sites in the United States, with almost 75% of sites considered tertiary care hospitals.”
Screening for lung cancer Sateia HF, Choi Y, Stewart RW, Peairs KS Semin Oncol. 2017 Feb;44(1):74-82. - “The incidence of lung cancer in the LDCT group was 645 cases per 100,000 person-years compared with lung cancer incidence in the CXR group of 572 cases per 100,000 person- years (rate ratio, 1.13; 95% CI, 1.03–1.23). The relative reduc- tion in lung cancer mortality with LDCT screening was 20.0% (95% CI, 6.8– 26.7; P 1⁄4 .004) over 5.4 years of follow up, with 247 lung cancer deaths per 100,000 person-years in the LDCT group and 309 deaths per 100,000 person-years in the CXR group.”
Screening for lung cancer Sateia HF, Choi Y, Stewart RW, Peairs KS Semin Oncol. 2017 Feb;44(1):74-82. - “The number needed to screen (NNS) to prevent one lung cancer death was 320. All-cause mortality was also decreased by 6.7% with a NNS of 219 to prevent one death.”
Screening for lung cancer Sateia HF, Choi Y, Stewart RW, Peairs KS Semin Oncol. 2017 Feb;44(1):74-82. - Limitations and Challenges of Screening
(1) the work up that ensues, one that may include invasive procedures that are potentially harmful especially in the case of a false positive result
(2) unnecessary treatment
(3) the anxiety it generates
(4) radiation exposure
(5) less inclination to quit
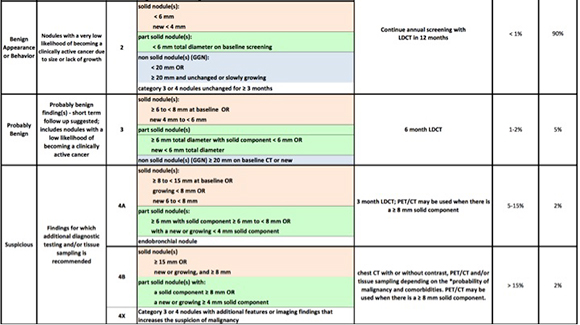
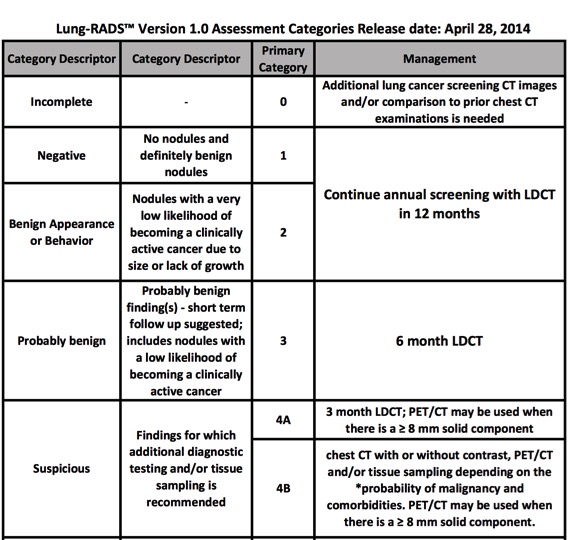
(6) cost - Lung Cancer Screening Guidelines
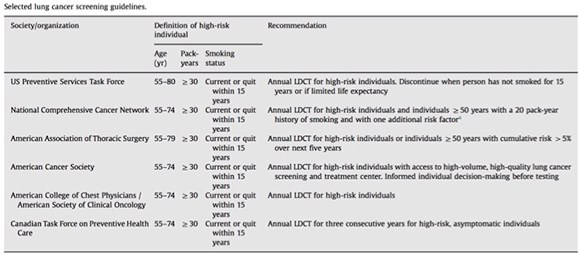
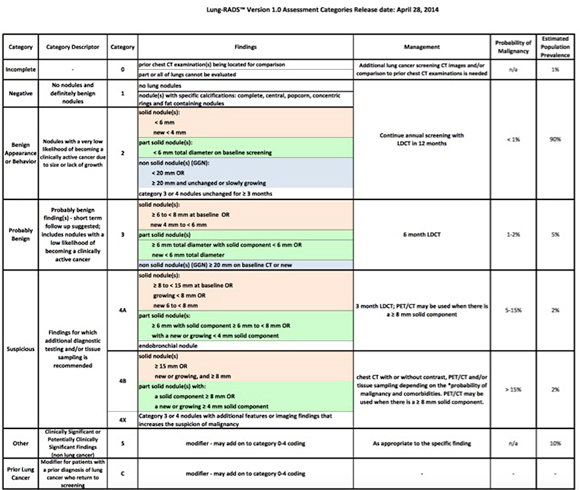
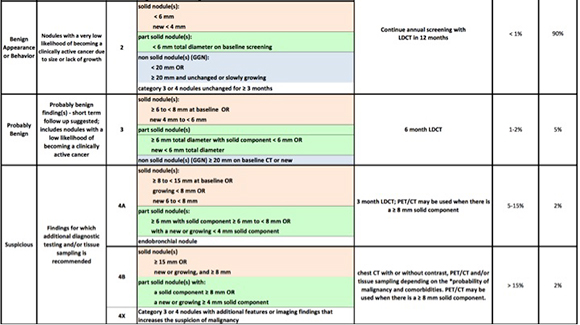
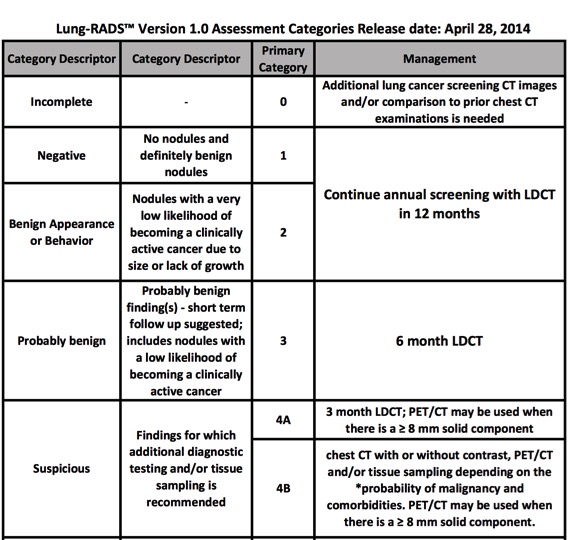
- “The ACR has developed a set of tools necessary for radiologists to take the lead on the front lines of lung cancer screening. The ACR Lung Cancer Screening Center designation is built upon the ACR CT accreditation program and requires use of Lung-RADS or a similar structured reporting and management system. This designation provides patients and referring providers with the assurance that they will receive high-quality screening with appropriate follow-up care.”
ACR CT Accreditation Program and the Lung Cancer Screening Program Designation Ella A. Kazerooni et al. JACR Vol 12, Issue 1, January 2015, Pages 38–42 - ACR Lung Cancer Screening Center designation: additional requirements
• Definition of eligible and appropriate screening population
• Incorporation of smoking cessation
• Physician qualification of at least 200 chest CT exams in the prior 36 months
• Structured reporting and management tool, such as Lung-RADS
• Multidetector, helical (spiral) scanner; low-dose CT protocol must have a CTDIvol of ≤3 mGy for a standard-size patient (5’7”; 154 lb)
• Exposure techniques must be adjusted for patient size
• Participation in the ACR Dose Index Registry is recommended
• Use and submit a low-dose CT protocol that meets the criteria outlined in the ACR- Society of Thoracic Radiology Practice Parameter for the Performance and Reporting of Lung Cancer Screening Thoracic CT - PURPOSE: The aim of this study was to assess the effect of applying ACR Lung-RADS in a clinical CT lung screening program on the frequency of positive and false-negative findings.
CONCLUSIONS: The application of ACR Lung-RADS increased the positive predictive value in our CT lung screening cohort by a factor of 2.5, to 17.3%, without increasing the number of examinations with false-negative results. Performance of ACR Lung-RADS in a Clinical
CT Lung Screening Program McKee BJ et al J Am Coll Radiol. 2016 Feb;13(2 Suppl):R25-9. - “ACR Lung-RADS reduced the overall positive rate from 27.6% to 10.6%. No false negatives were present in the 152 patients with >12-month follow-up reclassified as benign. Applying ACR Lung-RADS increased the positive predictive value for diagnosed malignancy in 1,603 patients with follow-up from 6.9% to 17.3%.”
Performance of ACR Lung-RADS in a Clinical CT Lung Screening Program McKee BJ et al J Am Coll Radiol. 2016 Feb;13(2 Suppl):R25-9. 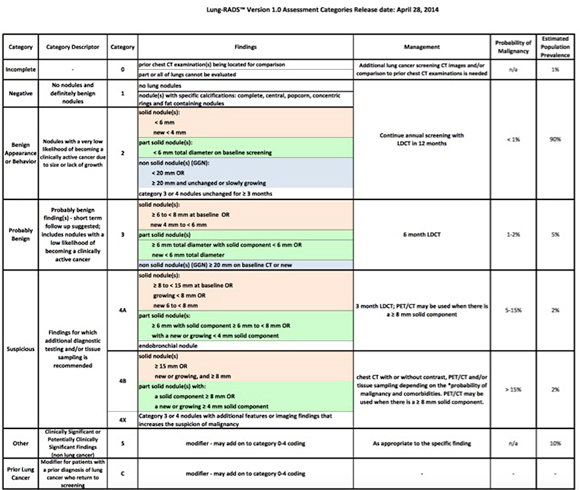
Colon
- Challenges for Virtual Colonoscopy
• Extra-colonic findings
• Potential of missing small expecially flat lesions
• Physican training for interpretation of the studies
• Physician acceptance of the procedure
• Cost of equipment
• Reimbursement - “Of the 11.7% (927/7952) of patients in our cohort with indeterminate or potentially significant extracolonic findings, 9.1% (725/7952) of findings were classified as E3 and 2.5% of findings (202/7952) were classified as E4; these figures are also consistent with prior studies .Because E4 findings are of the highest clinical suspicion, nearly all of these receive further workup or attention; further workup of E3 findings is substantialy more heterogeneous and is often subject to referring provider and patient preference.”
Extracolonic Findings at Screening CT Colonography: Prevalence, Benefits, Challenges, and Opportunities B. Dustin Pooler, David H. Kim, Perry J. Pickhardt AJR 2017; 209:1–9 - “Another key benefit of extracolonic evaluation at CTC that is often overlooked is the simple reassurance provided to the majority of patients (nearly 90%) for whom nothing of concern is found in the abdomen or pelvis. This negative information provides peace of mind that is rarely measured in research, but is nonetheless highly valued by patients.”
Extracolonic Findings at Screening CT Colonography: Prevalence, Benefits, Challenges, and Opportunities B. Dustin Pooler, David H. Kim, Perry J. Pickhardt AJR 2017; 209:1–9 - “Yet another potential bene t of extracolonic evaluation at CTC is the ability to provide opportunistic or synergistic screening for other conditions, most notably osteoporosis, as well as AAA and extracolonic cancer screening .”
Extracolonic Findings at Screening CT Colonography: Prevalence, Benefits, Challenges, and Opportunities B. Dustin Pooler, David H. Kim, Perry J. Pickhardt AJR 2017; 209:1–9 - “Although concern persists in some circles regarding the issue of extracolonic ndings at screening CTC, there is little in the literature to suggest that it causes substantial harm or has excessive cost, and a growing body of lit- erature suggests that there is additional value added in the form of detection of clinically significant disease and opportunities for additional screening outside the colon.”
Extracolonic Findings at Screening CT Colonography: Prevalence, Benefits, Challenges, and Opportunities B. Dustin Pooler, David H. Kim, Perry J. Pickhardt AJR 2017; 209:1–9 - “For those patients with E3 and E4 findings, a substantial percentage (20% overall and nearly 70% of E4 patients in our experience) will ultimately receive a diagnosis of previously unsuspected clinically relevant disease, typically requiring either treatment or surveillance. Most of the remaining cases will have benign conditions confirmed with either follow-up imaging or clinical follow-up alone, and less than 0.5% of all patients undergoing screening CTC will undergo invasive biopsy or surgery to prove a benign condition.”
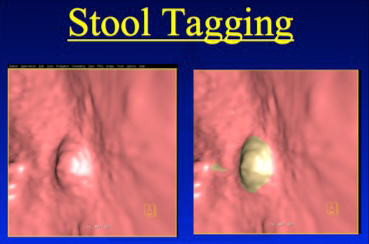
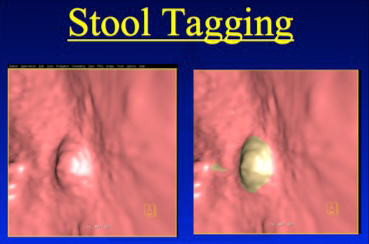
Extracolonic Findings at Screening CT Colonography: Prevalence, Benefits, Challenges, and Opportunities B. Dustin Pooler, David H. Kim, Perry J. Pickhardt AJR 2017; 209:1–9 - Virtual Colonoscopy Bowel Prep
• Diet
• Catharsis
- PEG (polyethylene glycol)
- Glycolax
- Magnesium citrate
• Tagging
- Barium
- Omnipaue-350 (50 cc before bedtime) - Johns Hopkins Prep Schedule
8AM
Clear liquid breakfast with 1 bottle barium.
Mix 4L PEG and put in Frig
Noon
Clear liquid lunch with 1/2 bottle of barium in 4 oz water
3PM
Drink 8 oz PEG every 15 minutes until gone (4-5 hours)
5PM
Drink 1/2 bottle barium in 4 oz
8PM
Take 2 bisacodyl tablets
Bedtime
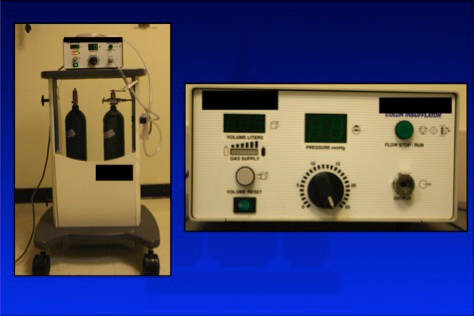
50cc Iohexol mixed in 8oz sprite - Colon Distension with CO2
Electronic CO2 insufflator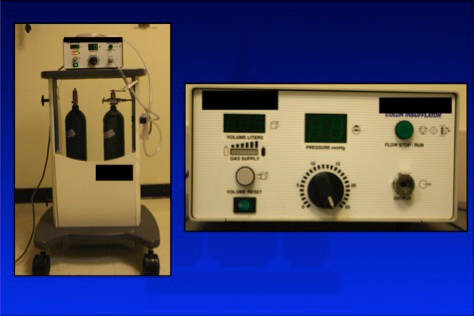
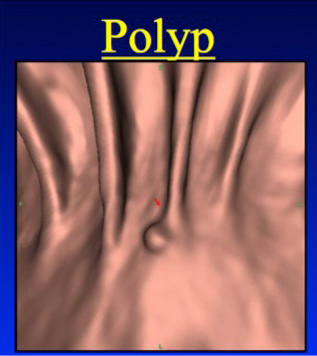
- Image Interpretation: 2D vs 3D
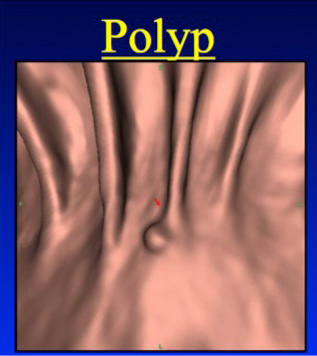
- Colon Polyps: Facts
• Polyps are common (60% men, 40% women at autopsy)
• Not all polyps are adenomas
• The prevalence of adenomas in the general population is 30-50% and increases with age
• Only 1-3% of all adenomas ever become malignant.
• It takes 10-15 years for an adenoma to become a carcinoma. - Colon Polyps : Who to Screen
• Estimated that approximately 12,000,000 adults per year in US are eligible for colorectal cancer screening
• High risk people at 40 (only represent 17% of patients who get colon cancer)
• High risk include FP, NFPCC, UC, Crohn, Family History
• Average risk people at 50 - Classic Colonoscopy: How Accurate is ir Really?
• Definitive procedure for evaluation of entire colon
– Requires sedation
– Risk of bleeding, perforation (1:1000), death (1-3:10,000)
• Completion rate 75-99% - anatomy & experience
– Polyps can be removed
• Misses 5-10% of adenomas > 1 cm.
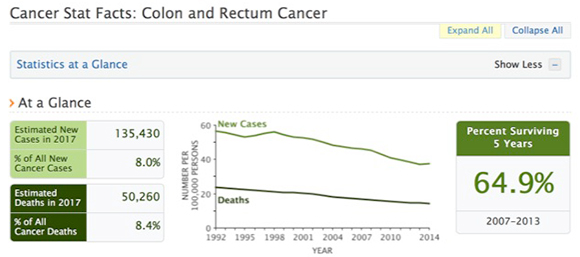
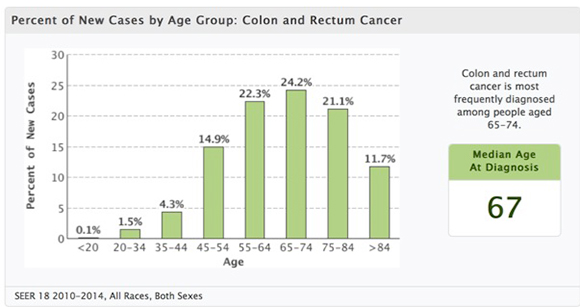
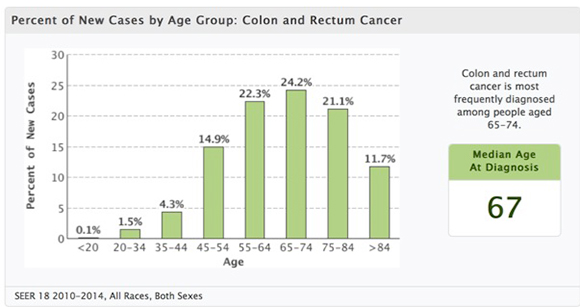
– Is it really necessary to remove tiny polyps? - SEER Data: Colon Cancer
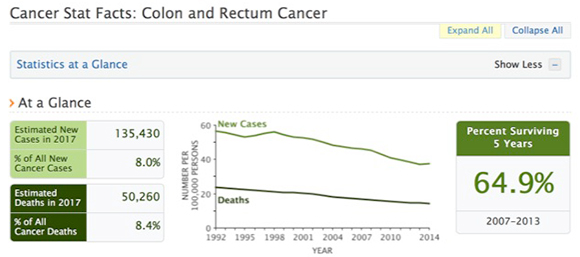
- SEER Data: Colon Cancer
- BACKGROUND: Advanced neoplasia represents the primary target for colorectal-cancer screening and prevention. We compared the diagnostic yield from parallel computed tomographic colonography (CTC) and optical colonoscopy (OC) screening programs.
CONCLUSIONS: Primary CTC and OC screening strategies resulted in similar detection rates for advanced neoplasia, although the numbers of polypectomies and complications were considerably smaller in the CTC group. These findings support the use of CTC as a primary screening test before therapeutic OC. CT colonography versus colonoscopy for the detection of advanced neoplasia.
Kim DH et al. N Engl J Med. 2007 Oct 4;357(14):1403-12.
Contrast
- “Extrinsic warming of room- temperature iodinated contrast material to human body temperature (37°C) is known to reduce contrast material viscosity, and results of some studies have shown that the practice can improve contrast material delivery rates with both hand and power injections through intravenous catheters.”
Rate of Contrast Material Extravasations and Allergic-like Reactions: Effect of Extrinsic Warming of Low-Osmolality Iodinated CT Contrast Material to 37° C Davenport MS et al. Radiology 2012; 262:475-484 - “Extrinsic warming of iodinated contrast material to 37°C reduces contrast ma- terial viscosity and has been advocated to decrease the frequency of adverse events related to intravenous administration and to improve iodinated contrast material delivery.”
Rate of Contrast Material Extravasations and Allergic-like Reactions: Effect of Extrinsic Warming of Low-Osmolality Iodinated CT Contrast Material to 37° C Davenport MS et al. Radiology 2012; 262:475-484
Deep Learning
- “The purpose of this review is to discuss developments in computational image analysis tools for predictive modeling of digital pathology images from a detection, segmentation, feature extraction, and tissue classification perspective. We discuss the emergence of new handcrafted feature approaches for improved predictive modeling of tissue appearance and also review the emergence of deep learning schemes for both object detection and tissue classification. We also briefly review some of the state of the art in fusion of radiology and pathology images and also combining digital pathology derived image measurements with molecular "omics" features for better predictive modeling. The review ends with a brief discussion of some of the technical and computational challenges to be overcome and reflects on future opportunities for the quantitation of histopathology.”
Image analysis and machine learning in digital pathology: Challenges and opportunities. Madabhushi A1, Lee G2. Med Image Anal. 2016 Oct;33:170-5
- “High-grade glioma is the most aggressive and severe brain tumor that leads to death of almost 50% patients in 1-2 years. Thus, accurate prognosis for glioma patients would provide essential guidelines for their treatment planning. Conventional survival prediction generally utilizes clinical information and limited handcrafted features from magnetic resonance images (MRI), which is often time consuming, laborious and subjective. In this paper, we propose using deep learning frameworks to automatically extract features from multi-modal preoperative brain images (i.e., T1 MRI, fMRI and DTI) of high-grade glioma patients. Specifically, we adopt 3D convolutional neural networks (CNNs) and also propose a new network architecture for using multi-channel data and learning supervised features.”
3D Deep Learning for Multi-modal Imaging-Guided Survival Time Prediction of Brain Tumor Patients. Nie D et al. Med Image Comput Comput Assist Interv. 2016 Oct;9901:212-220 - “While computerised tomography (CT) may have been the first imaging tool to study human brain, it has not yet been implemented into clinical decision making process for diagnosis of Alzheimer's disease (AD). On the other hand, with the nature of being prevalent, inexpensive and non-invasive, CT does present diagnostic features of AD to a great extent. This study explores the significance and impact on the application of the burgeoning deep learning techniques to the task of classification of CT brain images, in particular utilising convolutional neural network (CNN), aiming at providing supplementary information for the early diagnosis of Alzheimer's disease.”
Classification of CT brain images based on deep learning networks. Gao XW1, Hui R2, Tian Z Comput Methods Programs Biomed. 2017 Jan;138:49-56
- “This review covers computer-assisted analysis of images in the field of medical imaging. Recent advances in machine learning, especially with regard to deep learning, are helping to identify, classify, and quantify patterns in medical images. At the core of these advances is the ability to exploit hierarchical feature representations learned solely from data, instead of features designed by hand according to domain-specific knowledge. Deep learning is rapidly becoming the state of the art, leading to enhanced performance in various medical applications. We introduce the fundamentals of deep learning methods and review their successes in image registration, detection of anatomical and cellular structures, tissue segmentation, computer-aided disease diagnosis and prognosis, and so on.”
Deep Learning in Medical Image Analysis. Shen D, Wu G, Suk HI Annu Rev Biomed Eng. 2017 (in press)
- PURPOSE: Diabetic retinopathy (DR) is one of the leading causes of preventable blindness globally. Performing retinal screening examinations on all diabetic patients is an unmet need, and there are many undiagnosed and untreated cases of DR. The objective of this study was to develop robust diagnostic technology to automate DR screening. Referral of eyes with DR to an ophthalmologist for further evaluation and treatment would aid in reducing the rate of vision loss, enabling timely and accurate diagnoses.
CONCLUSIONS: A fully data-driven artificial intelligence-based grading algorithm can be used to screen fundus photographs obtained from diabetic patients and to identify, with high reliability, which cases should be referred to an ophthalmologist for further evaluation and treatment. The implementation of such an algorithm on a global basis could reduce drastically the rate of vision loss attributed to DR. Automated Identification of Diabetic Retinopathy Using Deep Learning. Gargeya R1, Leng T2. Ophthalmology. 2017 Mar 27. pii: S0161-6420(16)31774-2 - “In computerized detection of clustered microcalcifications (MCs) from mammograms, the traditional approach is to apply a pattern detector to locate the presence of individual MCs, which are subsequently grouped into clusters. Such an approach is often susceptible to the occurrence of false positives (FPs) caused by local image patterns that resemble MCs. We investigate the feasibility of a direct detection approach to determining whether an image region contains clustered MCs or not. Toward this goal, we develop a deepconvolutional neural network (CNN) as the classifier model to which the input consists of a large image window. The multiple layers in the CNN classifier are trained to automatically extract image features relevant to MCs at different spatial scales.”
Global detection approach for clustered microcalcifications in mammograms using a deep learning network. Wang J, Nishikawa RM, Yang Y J Med Imaging (Bellingham). 2017 Apr;4(2):024501
- “In summary, radiologists will not be replaced by machines. Radiologists of the future will be essential data scientists of medicine. We will leverage clinical data science and ML to diagnose and treat patients better, faster, and more efficiently. Although this new clinical data science milieu will undoubtedly alter radiology practice, if performed correctly, it will empower radiologists to continue to provide better actionable recommendations on the basis of new insights from the medical images and other relevant data.”
Big Data and Machine Learning—Strategies for Driving This Bus: A Summary of the 2016 Intersociety Summer Conference Kruskal JB et al. JACR (in press) - “Personalized predictive medicine necessitates the modeling of patient illness and care processes, which inherently have long-term temporal dependencies. Healthcare observations, stored in electronic medical records are episodic and irregular in time. We introduce DeepCare, an end-to-end deep dynamic neural network that reads medical records, stores previous illness history, infers current illness states and predicts future medical outcomes. At the data level, DeepCare represents care episodes as vectors and models patient health state trajectories by the memory of historical records.”
Predicting healthcare trajectories from medical records: A deep learning approach. Pham T et al. J Biomed Inform. 2017 May;69:218-229. - “Built on Long Short-Term Memory (LSTM), DeepCare introduces methods to handle irregularly timed events by moderating the forgetting and consolidation of memory. DeepCare also explicitly models medical interventions that change the course of illness and shape future medical risk.”
Predicting healthcare trajectories from medical records: A deep learning approach. Pham T et al. J Biomed Inform. 2017 May;69:218-229.
- “Medical images have unique issues that make radiology image interpretation more complex than it may first appear to non–domain-expert data scientists. The cost to develop data sets is very high, the process is fraught with legal issues, and, even in best case scenarios, the data sets will constitute only a fraction of the number of animal photos on Facebook and Instagram. A data set of images must be classified into relevant categories, such as “disease” and “normal.” This labor-intensive process depends on humans to classify the data. “
Ground truth” is the term for classification accuracy.” Big Data and Machine Learning—Strategies for Driving This Bus: A Summary of the 2016 Intersociety Summer Conference Kruskal JB et al. JACR (in press) - “Historically, the limiting factor to useful ML projects has been appropriate training data sets. For the moment, at least, radiologists hold great power over the imaging, clinical, and radiology-expertise data needed to develop image interpretation deep learning algorithms. This data combination is hugely valuable. When these algorithms finally do arrive, they have the potential to disrupt radiology adversely.”
Big Data and Machine Learning—Strategies for Driving This Bus: A Summary of the 2016 Intersociety Summer Conference Kruskal JB et al. JACR (in press) - “Whether small or large, good data sets for ML are complex, expensive undertakings. Data sets must be partitioned into training, verification, and validation portions; some of these data will be part of the public domain, whereas other data would be private. Large data sets aggregated from multiple sources face issues including intellectual property (IP), business agreements, and governance, all of which need to be resolved.”
Big Data and Machine Learning—Strategies for Driving This Bus: A Summary of the 2016 Intersociety Summer Conference Kruskal JB et al. JACR (in press) - “Moving up to the health state level, historical and present health states are then aggregated through multiscale temporal pooling, before passing through a neural network that estimates future outcomes. We demonstrate the efficacy of DeepCare for disease progression modeling, intervention recommendation, and future risk prediction. On two important cohorts with heavy social and economic burden - diabetes and mental health - the results show improved prediction accuracy.”
Predicting healthcare trajectories from medical records: A deep learning approach. Pham T et al. J Biomed Inform. 2017 May;69:218-229.
- “Although more medical information than ever is now contained within EHRs, data continue to exist in isolated silos. Appropriate data analytic tools are imperative to handle disparate data and mine these data efficiently and usefully. Owning the clinical and imaging follow-up loops is necessary to cement our clinical relevance.”
Big Data and Machine Learning—Strategies for Driving This Bus: A Summary of the 2016 Intersociety Summer Conference Kruskal JB et al. JACR (in press)
- “The authors demonstrated that the DL-CNN can overcome the strong boundary between two regions that have large difference in gray levels and provides a seamless mask to guide level set segmentation, which has been a problem for many gradient-based segmentation methods. Compared to our previous CLASS with LCR method, which required two user inputs to initialize the segmentation, DL-CNN with level sets achieved better segmentation performance while using a single user input. Compared to the Haar-feature-based likelihood map, the DL-CNN-based likelihood map could guide the level sets to achieve better segmentation. The results demonstrate the feasibility of our new approach of using DL-CNN in combination with level sets for segmentation of the bladder.”
Urinary bladder segmentation in CT urography using deep-learning convolutional neural network and level sets. Cha KH et al. Med Phys. 2016 Apr;43(4):1882
Liver
- “FNH is a benign hypervascular tumor arising from the normal liver parenchyma. It occurs - FNH are a central scar, intratumoral centrifugal arteries from the center, and the presence of Kupffer cells and the proliferation of cholangiole, among others.
On contrast-enhanced CT, FNHs undergo marked enhancement during the arterial phase, becoming appreciably hyperattenuating relative to the hepatic parenchyma. Moreover, one or more large feeding hepatic arteries, small central and septal arteries, and early draining veins.”
Hypervascular Benign and Malignant Liver Tumors That Require Differentiation from Hepatocellular Carcinoma: Key Points of Imaging Diagnosis Takamichi Murakami* and Masakatsu Tsurusaki Liver Cancer. 2014 May; 3(2): 85–96.
- “This educational review focuses on the epidemiology and radiological evaluation of the various subtypes of hepatic adenomas (HCAs). It includes detailed discussion of the imaging appearances of each HCA subtype and the clinical relevance of the new classification system. Each HCA subtype has a unique biological behaviour. Imaging plays a central role in diagnosis, subtype characterisation, identification of complications, and follow-up assessment. Management of patients should vary according to the specific HCA subtype.”
Hepatocellular adenoma: imaging review of the various molecular subtypes. Dharmana H1, Saravana-Bawan S2, Girgis S3, Low G2. Clin Radiol. 2017 Apr;72(4):276-285 - “The exact mechanism for malignant transformation into HCCs is not well understood. Rapid increase in the size of a previously stable HCA raises the possibility of malignant degeneration or haemorrhage. A recent systematic review by Stoot et al. found that the incidence of malignant transformation was approximately 4.2%. The β-catenin activated subtype has the highest predilection for malignant transformation of all HCAs..”
Hepatocellular adenoma: imaging review of the various molecular subtypes. Dharmana H1, Saravana-Bawan S2, Girgis S3, Low G2. Clin Radiol. 2017 Apr;72(4):276-285 - “HCA has been described in patients with glycogen storage disorders (GSDs), particularly type 1 (Von Gierke's disease) and type 3.GSDs are hereditary disorders with an autosomal recessive transmission. They are characterised by abnormal glycogen accumulation in the liver, which causes chronic inflammation and predisposes to HCA development. HCAs associated with GSDs commonly affect males (male to female ratio of 2:1) and typically develop in patients <20 years of age.These HCAs are more likely to be multiple and have a higher risk of malignant transformation into HCC.”
Hepatocellular adenoma: imaging review of the various molecular subtypes. Dharmana H1, Saravana-Bawan S2, Girgis S3, Low G2. Clin Radiol. 2017 Apr;72(4):276-285 - “Metastatic liver tumor of adenocarcinoma, such as colon cancer or pancreatic cancer, often shows doughnut-like ring enhancement due to its mucinous and fibrous components. As a result, it needs to be differentiated from cholangiocarcinoma. Metastatic liver tumors of renal cell carcinoma, breast cancer, and neuroendocrine tumors, for example, exhibit hypervascularity and have to be differentiated from HCC. When the primary lesion is known, metastatic tumors can be easily diagnosed.”
Hypervascular Benign and Malignant Liver Tumors That Require Differentiation from Hepatocellular Carcinoma: Key Points of Imaging Diagnosis Takamichi Murakami* and Masakatsu Tsurusaki Liver Cancer. 2014 May; 3(2): 85–96.
Pancreas
- “Despite published guidance recommendations and reported awareness of them, fewer than half of follow-up recommendations for FCPL are consistent with the guidance and considerable variability persists among radiologists.”
Focal Cystic Pancreatic Lesion Follow-up Recommendations After Publication of ACR White Paper on Managing Incidental Findings Mark D. Bobbin et al. J Am Coll Radiol 2017 (in press) - “Nonadherence to management recommendations among our radiologists was particularly notable in the subset of cases in which no follow-up recommendation was made. Just over 40% of reports correctly followed ACR guidance by not providing a follow-up recommendation. Based on the algorithm, however, our radiologists should have provided a follow-up recommendation in almost 60% of this sample.”
Focal Cystic Pancreatic Lesion Follow-up Recommendations After Publication of ACR White Paper on Managing Incidental Findings Mark D. Bobbin et al. J Am Coll Radiol 2017 (in press) - “Radiologists may favor providing follow-up recommendations that more closely reflect the manage- ment algorithm preferred by ordering providers rather than those provided by outside organizations.”
Focal Cystic Pancreatic Lesion Follow-up Recommendations After Publication of ACR White Paper on Managing Incidental Findings Mark D. Bobbin et al. J Am Coll Radiol 2017 (in press)
- “Neoplastic and inflammatory diseases that can closely simulate pancreatic adenocarcinoma include neuroendocrine tumor, metastasis to the pancreas, lymphoma, groove pancreatitis, autoimmune pancreatitis, and focal chronic pancreatitis. Atypical imaging findings that should suggest diagnoses other than adenocarcinoma include the absence of significant duct dilatation, incidental detection, hypervascularity, large size (> 5 cm), IV tumor thrombus, and intralesional ducts or cysts.”
Pancreatic Imaging Mimics: Part 1, Imaging Mimics of Pancreatic Adenocarcinoma Fergus V. Coakley et al. American Journal of Roentgenology. 2012;199: 301-308
Practice Management
- “The health care industry has recognized the importance of the patient experience. We believe that the biggest driver of patient experience is medical staff experience. If we want to increase patient experience, we must first improve the experience of the medical staff and providers.”
Transforming the Health Care Experience: Doctors, Nurses, Patients, and Beyond Trina Spear, Karen M. Horton, Elliot K. Fishman, Pamela T. Johnson, Journal of the American College of Radiology (in press) - “What we found through our work with hospitals around the country is that when patients walk into a hospital where each department is color coded by group, the hospital logo is embroidered on every top, and all the scrubs and laboratory coats are well fitted and pressed, it changes how they think about the institution. From the patients’ perspective, they trust the doctors and nurses, and their opinions of the providers’ performance improve exponentially.”
Transforming the Health Care Experience: Doctors, Nurses, Patients, and Beyond Trina Spear, Karen M. Horton, Elliot K. Fishman, Pamela T. Johnson, Journal of the American College of Radiology (in press) - “Many patients are visiting your department for the first time. Their confidence in the quality of the care you deliver will be influenced by the appearance of your physicians, house staff, nurses, and technologists. Making sure the “uniform” is a quality presentation may improve patients’ perceptions of your department’s and institution’s quality. The proper dress code may have positive unintended consequences. On the other hand, if the point of contact to the providing care team is poorly dressed (ie, wrinkled or poorly fitting scrubs), patients may
become concerned about the entire operation.”
Transforming the Health Care Experience: Doctors, Nurses, Patients, and Beyond Trina Spear, Karen M. Horton, Elliot K. Fishman, Pamela T. Johnson, Journal of the American College of Radiology (in press)
Small Bowel
- Treatment
• Surgical resection is mainstay therapy for isolated small tumors without evidence of metastatic disease.
• Laparoscopic resection may be attempted for small tumors with open procedures reserved for larger tumors.
• Imatinib mesylate, a tyrosine kinase inhibitor, is first line therapy for patients who are poor surgical candidates, or show evidence of recurrence or metastatic disease.
• Can also be used as neoadjuvant therapy to preoperatively shrink large tumors - Imaging Surveillance
• Surveillance after surgery includes CT scanning with contrast every 3 to 6 months.
• Low grade small tumor may have scans every 6 to 12 months.
• Patients receiving imatinib mesylate therapy may have scans every 3 months.
• Dual phase imaging is recommended as arterial phase may detect new enhancing components in stable disease that may wash out during venous phase and be overlooked.
- Lymphoma of the Small Bowel: Facts
• Third most common small bowel malignancy.
• Inflammatory bowel disease and history of solid organ transplantation are known risk factors
• Stomach is the most common site of gastrointestinal tract involvement followed by ileum
• Infiltrating mildly enhancing mass ± regional lymphadenopathy and splenomegaly. Classic “aneurysmal bowel dilatation” appearance of affected segment.
• Non-Hodgkin B-cell lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma) is the most common subtype
- Small Bowel Angiodysplasia: Facts
• Most common cause of small bowel bleeding
• Associated with end-stage renal disease and aortic stenosis
• Most common in the right colon but can occur throughout the small bowel
• Tuft -like hypervascular enhancing focus less than 5 mm which fades on delayed phases.
• Multifocal in 40% to 75% cases
• Composed of abnormally dilated thin-walled vessels with high propensity for bleeding
- Small Bowel Carcinoid Tumors: Facts
• Second most common small bowel malignancy.
• Rarely presents with carcinoid syndrome (watery diarrhea, flushing and endocardial fibrosis) when disease spreads to the liver
• Appendix most common site followed by ileum
• Avidly enhancing polypoid mass.
• Primary tumor usually small.
• Tumor spread with calcified mesenteric mass with desmoplastic response and tethering of adjacent small bowel loops.
• Liver metastasis usually hypervascular
- Small Bowel GIST Tumors: Facts
• Most common mesenchymal tumor of the gastrointestinal tract.
• Increased incidence in NF-1 patients
• Most common in the stomach followed by small bowel
• May present as GI bleed when the lesions are smaller and the tumor very vascular
• Larger tumors are usually of higher grade than smaller tumors - GIST Tumors of the Small Bowel:
Clinical Presentation
• bowel obstruction
• intraluminal GI bleeding (occult or frank) from mucosal ulceration
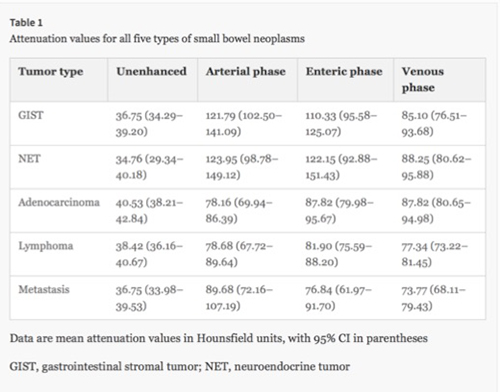
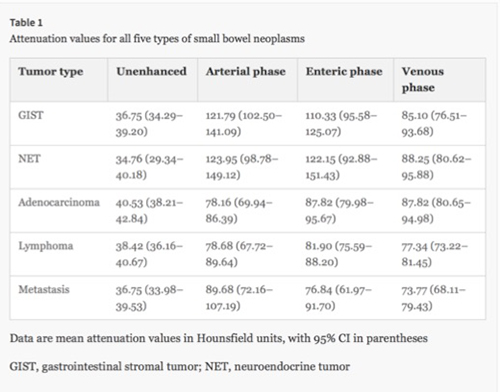
• intraperitoneal bleeding secondary to rupture - Small Bowel Tumors:CT Attenuation
- “They are typically well-circumscribed tumors and usually arise from the muscularis propria of the gastrointestinal tract. The classic tendency is for exophytic growth, especially since they arise from the outer muscular layer. There is usually some growth towards the lumen however, as up to 50% of GISTs will exhibit mucosal ulceration on the luminal surface.”
Getting the GIST: a pictorial review of the various patterns of presentation of gastrointestinal stromal tumors on imaging Scola D, Bahoura L, Copelan A. et al. Abdom Radiol (2017) 42: 1350-1364 - “The size of tumors is highly variable, ranging from several millimeters to greater than 30 cm; the median tumor size for those considered high-risk (e.g., locally advanced primary tumor or metastatic/recurrent tumor) is reported as 8.9 cm .”
Getting the GIST: a pictorial review of the various patterns of presentation of gastrointestinal stromal tumors on imaging Scola D, Bahoura L, Copelan A. et al. Abdom Radiol (2017) 42: 1350-1364 - “Up to 30% of GISTs have poor prognostic factors including size >5 cm, lobulated contour, heterogeneous enhancement, presence of mesenteric fat infiltration, ulceration, regional lymphadenopathy or an exophytic growth pattern on CT .”
Getting the GIST: a pictorial review of the various patterns of presentation of gastrointestinal stromal tumors on imaging Scola D, Bahoura L, Copelan A. et al. Abdom Radiol (2017) 42: 1350-1364 - “They most commonly arise in the stomach (approximately 60%), followed by the jejunum/ileum (30%), duodenum (5%), colon (4%), and esophagus or appendix (1%). Even more rare are primary extra-intestinal locations. Clinical presentations are highly variable and usually dependent on tumor size and location .”
Getting the GIST: a pictorial review of the various patterns of presentation of gastrointestinal stromal tumors on imaging Scola D, Bahoura L, Copelan A. et al. Abdom Radiol (2017) 42: 1350-1364 - “GISTs occurring in the duodenum and remainder of the small bowel can also demonstrate any growth pattern but are commonly exophytic, possibly explained by slow growth and often delayed presentations. Calcifications are uncommon but can occasionally be present within larger GISTs. When large, enhancement is often heterogeneous, and there can be large hypo-attenuating necrotic components. They can also be arterially hyper-enhancing.”
Getting the GIST: a pictorial review of the various patterns of presentation of gastrointestinal stromal tumors on imaging Scola D, Bahoura L, Copelan A. et al. Abdom Radiol (2017) 42: 1350-1364 - “If a tumor is larger than 5 cm, and if removal would result in excessive damage to surrounding structures, it is typically considered unresectable. In these instances, treatment with targeted therapy (such as imatinib mesylate) is performed. Because mutational activation of TK receptors (KIT or PDGFRA) stimulates growth, targeted therapy agents are tyrosine kinase inhibitors, selectively blocking the GIST’s growth signal. Targeted therapy after surgical resection has become the standard of care to help prevent recurrence or treat recurrence or metastatic disease.”
Getting the GIST: a pictorial review of the various patterns of presentation of gastrointestinal stromal tumors on imaging Scola D, Bahoura L, Copelan A. et al. Abdom Radiol (2017) 42: 1350-1364 - “Imaging evaluation of GISTs tumors using rapid reduction in size to indicate treatment response to target therapies can be used as in the Response Evaluation Criteria in Solid Tumors (RECIST) criteria . In these instances rapid decrease in tumor size and number of lesions has been described. However size criteria alone underestimates/misinterprets good response, as stable or initially increasing size has been described . FDG PET can increase accuracy of RECIST criteria by showing decreasing FDG-avidity over time.”
Getting the GIST: a pictorial review of the various patterns of presentation of gastrointestinal stromal tumors on imaging Scola D, Bahoura L, Copelan A. et al. Abdom Radiol (2017) 42: 1350-1364 - “The most frequent clinical indication for imaging, which led to detection of the small bowel GISTs in our series, was suspected small bowel bleeding (45/111; 40.5%), with 34/45 of these patients having (75.5%) overt and 11/45 (24.5%) having occult small bowel bleeding. Abdominal pain was the indication for imaging in slightly over one-third of patients (41/111; 37%), with cancer surveillance in asymptomatic patients accounting for 9% (10/111) and clinical suspicion for potential small bowel tumor in 13% (15/111).”
Impact of CT enterography on the diagnosis of small bowel gastrointestinal stromal tumors Vasconcelos, R.N., Dolan, S.G., Barlow, J.M. et al. Abdom Radiol May 2017, Volume 42, Issue 5, pp 1365–1373
- OBJECTIVE: Lower gastrointestinal hemorrhage is a common cause of hospitalization and has substantial associated morbidity and financial cost. CT angiography (CTA) is emerging as an alternative to (99m)Tc-labeled RBC scintigraphy (RBC scintigraphy) for the localization of acute lower gastrointestinal bleeding (LGIB); however, data on comparative efficacy are scant. The aim of this study was to assess the utility of CTA compared with RBC scintigraphy in the overall evaluation and management of acute LGIB.
Localizing Acute Lower Gastrointestinal Hemorrhage: CT Angiography Versus Tagged RBC Scintigraphy. Feuerstein JD et al. AJR Am J Roentgenol. 2016 Sep;207(3):578-84 - CONCLUSION:
Both CTA and RBC scintigraphy can be used to identify active bleeding in 38% of cases. However, the site of bleeding is localized with CTA in a significantly higher proportion of studies.
Localizing Acute Lower Gastrointestinal Hemorrhage: CT Angiography Versus Tagged RBC Scintigraphy. Feuerstein JD et al. AJR Am J Roentgenol. 2016 Sep;207(3):578-84 - MATERIALS AND METHODS: We retrospectively reviewed images from all CTA examinations performed for suspected acute LGIB at our tertiary care hospital from January 2010 through November 2011. The comparison group was determined by retrospective review of twice the number of RBC scintigraphic scans consecutively obtained from June 2008 to November 2011 for the same indication. All CTA and RBC scintigraphic scans were reviewed for accurate localization of the site and source of suspected active LGIB.
Localizing Acute Lower Gastrointestinal Hemorrhage: CT Angiography Versus Tagged RBC Scintigraphy. Feuerstein JD et al. AJR Am J Roentgenol. 2016 Sep;207(3):578-84 - “Seventeen (38%) CTA scans showed active gastrointestinal bleeding compared with 34 (38%) RBC scintigraphic scans (p = 1.000). However, the site of bleeding was accurately localized on 24 (53%) CTA scans. This proportion was significantly greater than the proportion localized on RBC scintigraphic scans (27 [30%]) (p = 0.008).”
Localizing Acute Lower Gastrointestinal Hemorrhage: CT Angiography Versus Tagged RBC Scintigraphy. Feuerstein JD et al. AJR Am J Roentgenol. 2016 Sep;207(3):578-84 - “Our data strongly support CTA as a valuable addition to the current modalities for the evaluation and management of acute LGIB. We expect that future studies with a larger sample size and a prospective design will con- firm our findings and help establish CTA as the preferred imaging modality in the overall algorithm for the management of acute LGIB.”
Localizing Acute Lower Gastrointestinal Hemorrhage: CT Angiography Versus Tagged RBC Scintigraphy. Feuerstein JD et al. AJR Am J Roentgenol. 2016 Sep;207(3):578-84 - PURPOSE: To evaluate the negative predictive power of computed tomography angiography (CTA) for the identification of obscure acute gastrointestinal (GI) bleeding (GI bleeding not visualized/treated by endoscopy) on subsequent mesenteric angiography (MA) with the intention to treat.
CONCLUSIONS: The high NPV of CTA for the evaluation of GI bleeding suggests utility for excluding patients that are unlikely to benefit from MA and subsequent endovascular therapy. CTA may be considered for the first line diagnostic study for the evaluation of obscure GI bleeding.
Localizing Acute Lower Gastrointestinal Hemorrhage: CT Angiography Versus Tagged RBC Scintigraphy. Feuerstein JD et al. AJR Am J Roentgenol. 2016 Sep;207(3):578-84 - Lower GI Bleeding: Facts
• lower gastrointestinal bleeding (LGIB) accounts for approximately 24% of cases of gastrointestinal hemorrhage
• The disease spectrum varies from chronic and intermittent blood loss to severe acute hemorrhage.
• Overall mortality ranges from 4% to 5% but can be as high as 23% depending on age, comorbid conditions, and severity of hemorrhage
- “Right lower quadrant pain is one of the most common indications for imaging evaluation of the abdomen in the emergency department setting. This article reviews important imaging findings associated with acute appendicitis as well as major differential considerations including: mesenteric adenitis, Meckel diverticulum, neutropenic colitis, right-sided diverticulitis, epiploic appendagitis, omental infarction, and inflammatory bowel diseaseRight lower quadrant pain is one of the most common indications for imaging evaluation of the abdomen in the emergency department setting. This article reviews important imaging findings associated with acute appendicitis as well as major differential considerations including: mesenteric adenitis, Meckel diverticulum, neutropenic colitis, right-sided diverticulitis, epiploic appendagitis, omental infarction, and inflammatory bowel disease.”
Evaluating the Patient with Right Lower Quadrant Pain. Patel NB, Wenzke DR. Radiol Clin North Am. 2015 Nov;53(6):1159-70
Vascular
- BACKGROUND: Multidetector computed tomography angiography (MDCTA) and magnetic resonance angiography (MRA) are accurate techniques for selecting patients with peripheral arterial disease for surgical and endovascular treatment. No studies in the literature have directly compared MDCTA and MRA to establish which one should be employed, in patients suitable for both techniques, before endovascular treatment.
CONCLUSION: Our results suggest that MDCTA can be considered as a first-line investigation in patients being candidates for endovascular procedures when clinical history or duplex sonographic evaluation are indicative of severe impairment of the infrapopliteal segment.
Comparison of CT and MR angiography in evaluation of peripheral arterial disease before endovascular intervention. Cina A et al. Acta Radiol. 2016 May;57(5):547-56. - RESULTS: MDCTA and MRA accurately classify disease in the aorto-iliac (accuracy 0.92 for MDCTA and MRA) and femoro-popliteal (MDCTA 0.94, MRA 0.90) segments. MDCTA was more accurate in stratifying disease in the infrapopliteal segments (0.96 vs. 0.9) and in assessing the impairment of runoff arteries (0.92 vs. 0.85) at per-segment analysis. MDCTA showed a higher confidence and a shorter examination time.
Comparison of CT and MR angiography in evaluation of peripheral arterial disease before endovascular intervention. Cina A et al. Acta Radiol. 2016 May;57(5):547-56.