MDCT Review of Intravenous Drug Abuse ComplicationsMDCT Review of Intravenous Drug Abuse Complications Franco Verde, MD |
Disclosures None of the authors have any relevant disclosures |
Outline
|
Introduction
|
Introduction
|
Introduction
|
Introduction
|
Cutaneous Infections
|
Manifestations on Imaging
|
Superficial Complications Figure 1. 32 year old woman with history of intravenous drug use presents with inguinal pain and drainage for the past few days after attempting to inject heroin. IV contrast enhanced CT images of the pelvis with axial (A) and sagittal reconstruction (B) demonstrates skin thickening and subcutaneous fat stranding at the site of injection (A, B, yellow arrows). Few foci of gas (B, red arrow) are present from injection. Note the track of the fat stranding to the level of the femoral vessels (*) on the axial image. 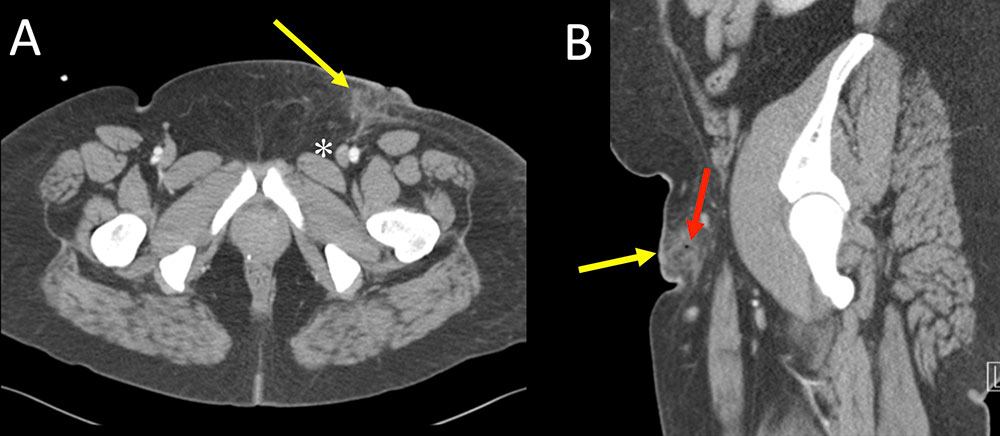 |
Superficial Complications Figure 2. 33 year old man with history of intravenous drug use presenting for hand pain 5 days after injecting cocaine. Physical exam and bedside ED sonogram was suspicious for hand abscess. IV contrast enhanced CT images of the hand with axial (A), coronal (B) and full volume 3D rendering (C) demonstrates subtle rim-enhancing abscess (A,B, orange arrows) measuring 1.7 cm. Volume rendering demonstrates focal swelling within the first webspace (C, yellow arrow). 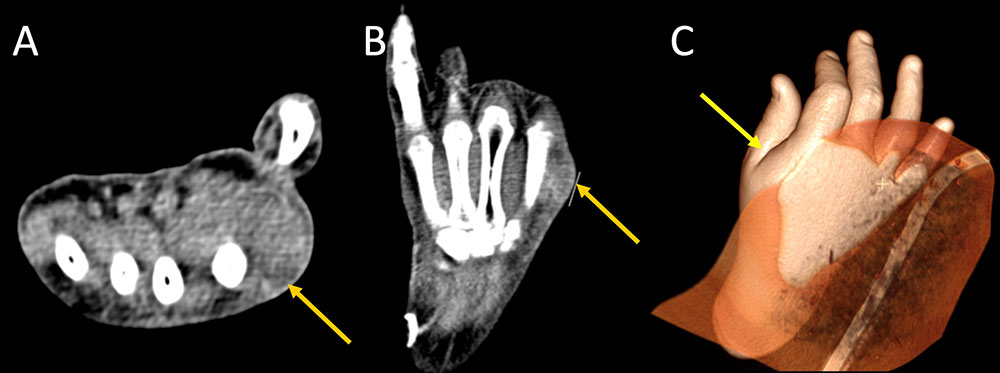 |
Superficial Complications Figure 3. 53 year old man with history of intravenous drug use and skin popping presents with a week of shoulder and upper arm pain after injecting heroin. IV contrast enhanced CT images of the right upper extremity with axial (A), coronal (B) and full volume 3D rendering (C) demonstrates a large rim-enhancing abscess involving the deltoid muscle (A,B, yellow arrows) measuring 6 x 4 cm in transverse dimension extending up to 7 cm in craniocaudal dimension. 3D volume rendering demonstrates an obvious region of focal swelling at site of abscess (C, red arrow). 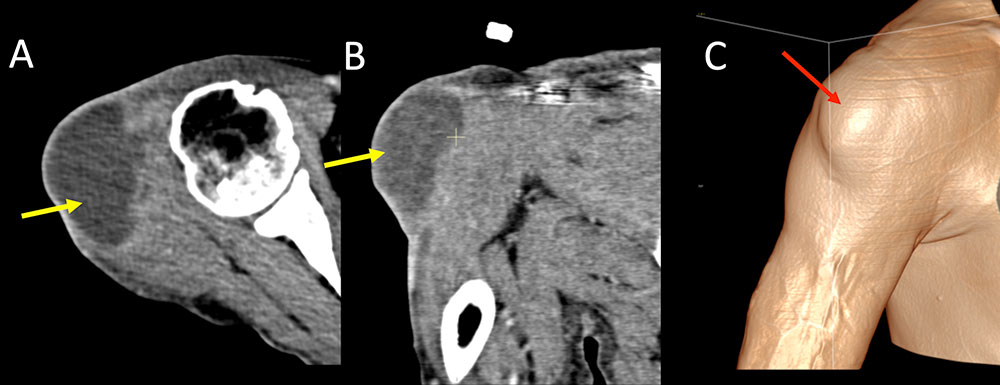 |
Superficial Complications Figure 4. 55 year old man with a history of intravenous drug use and skin popping presents with a week of shoulder and upper arm pain after injecting heroin. IV contrast enhanced CT images of the left upper extremity with axial (A), coronal (B) and full volume 3D rendering (C) demonstrates a large, irregular, insinuating, rim-enhancing abscess involving the anterior compartment of the upper arm (A,B, yellow arrows) extending from the subacromial region to mid humerus, measuring 6 x 6 cm in axial dimension and extending for up to 19 cm in craniocaudal dimension. Volume rendering demonstrates an marked regional swelling at site of abscess (C, red arrow). 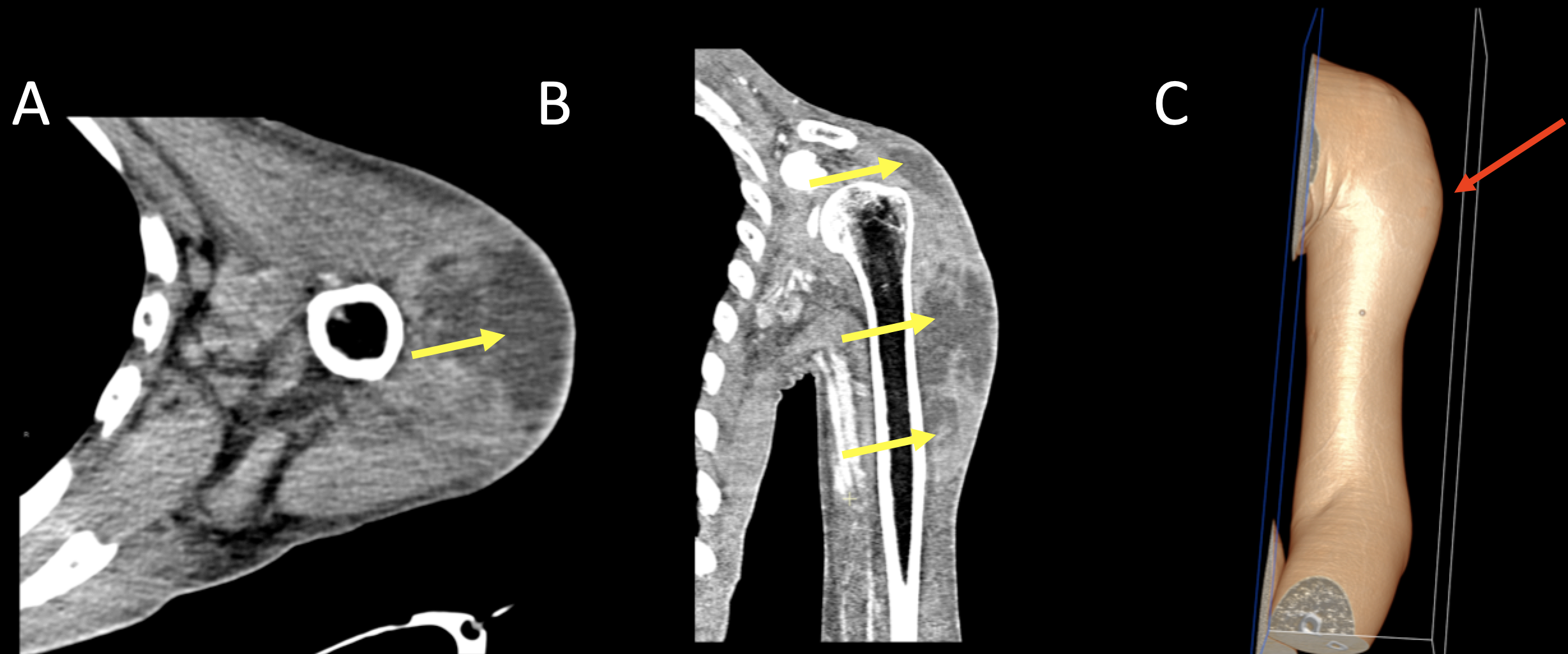 |
Superficial Complications Figure 5. 55 year old woman with long history of intravenous drug use, HIV/AIDS, hepatitis C, presents with increasing neck pain and swelling after injecting into the right neck 3 days ago. IV contrast enhanced CT in axial (A) and coronal (B, C) planes demonstrates a large 5 x 8 x 10 cm multiloculated abscess within the right supraclavicular region (A, B, C red arrows). Note the broken retained needle fragment from injection (B, yellow arrow). Patient was admitted to surgery for emergent debridement. 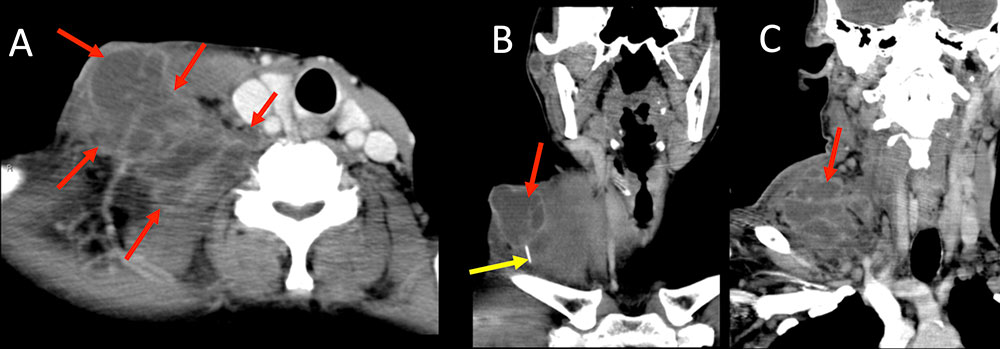 |
Deeper Infections
|
Deeper Infections
|
Deeper Complications Figure 5. 35 year old man with history of intravenous drug use sent to ED by police (after being arrested for other reasons) for evaluation of open arm wound. Patient endorses wound was present for the past 3 to 4 months. IV contrast enhanced CT of the upper extremity demonstrates a large open wound (A, B, red arrows) with advanced osteomyelitis of the radius and ulna (A, yellow arrow). Volume rendering allows full appreciation of wound extent for the radiologist. One must be careful not to confuse the clip plane (B, red arrowhead) used to create the 3D image for additional pathology. 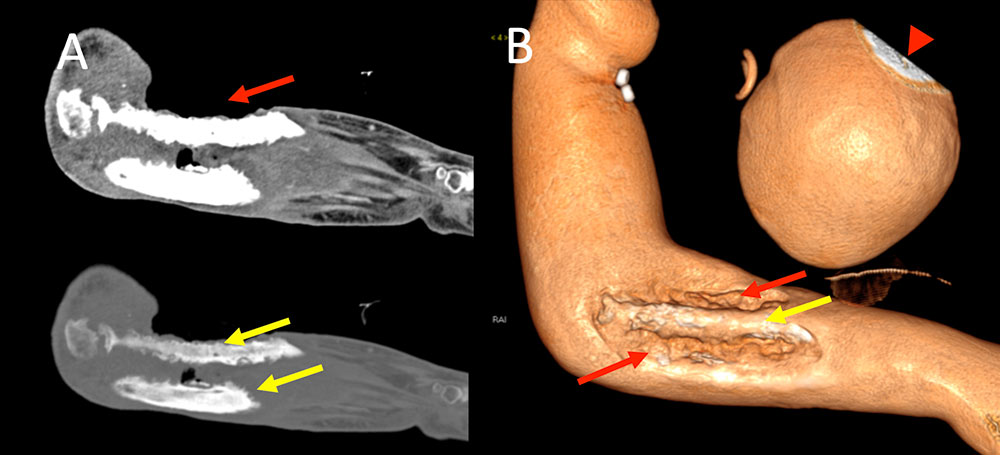 |
Deeper Complications Figure 6. 23 year old woman with history of intravenous drug use presents to ED with increasing leg, groin, and pelvic pain. Patient has a fever with leukocytosis. IV contrast enhanced CT imaging in sequential axial plane (A) demonstrates large amount of left inguinal inflammation (A, yellow arrows) with developing abscesses (A, red arrows). Additional edema noted through left psoas muscle. Oblique coronal MPR (B) well demonstrates full extent of abscesses and edema (B, red and yellow arrows). 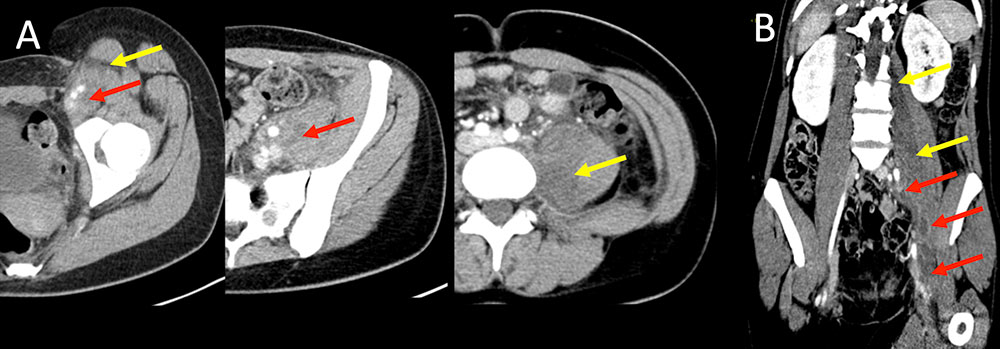 |
Vascular Complications
|
Vascular Complications Figure 7. 41 year old woman with history of intravenous drug use presents with leg pain after injecting cocaine into her legs. Axial (A) and coronal (B) IV contrast enhanced CT of the lower extremities demonstrates asymmetric skin thickening and subcutaneous fat stranding, compatible with cellulitis (A, B yellow arrows). Adjacent dilated venous structures are noted (A, B red arrows). Doppler analysis of the area demonstrates tubular dilated structure without blood flow (C, red arrow). Findings are compatible with superficial thrombophlebitis from direct injection. 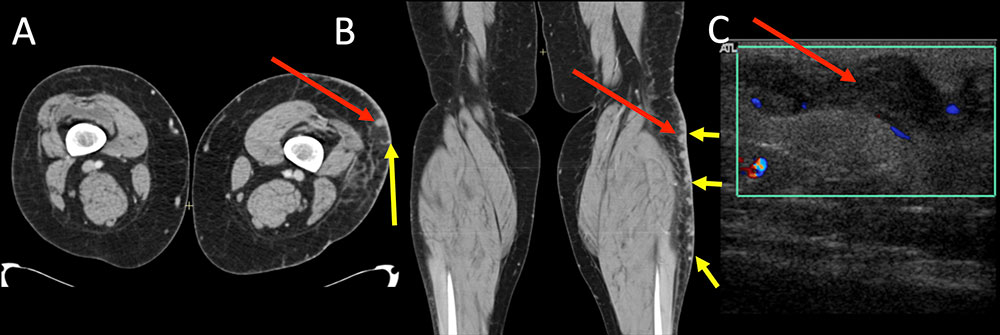 |
Vascular Complications Figure 8. 47 year old woman with history of intravenous drug use presents for severe groin pain. Axial IV contrast enhanced CT of the pelvis and upper thigh (A) demonstrates three saccular pseudoaneurysms arising from the right common and proximal femoral arteries. Largest pseudoaneurysm measures 1.6 x 1.4 cm and smallest measures 0.8 cm (A, B, red arrows). Surrounding hematoma is also present (A, B, yellow arrows). Coronal MPR (B) and MIP images (C) fully depict all the pseudoaneurysms in a single image which may be helpful for vascular surgical planning. 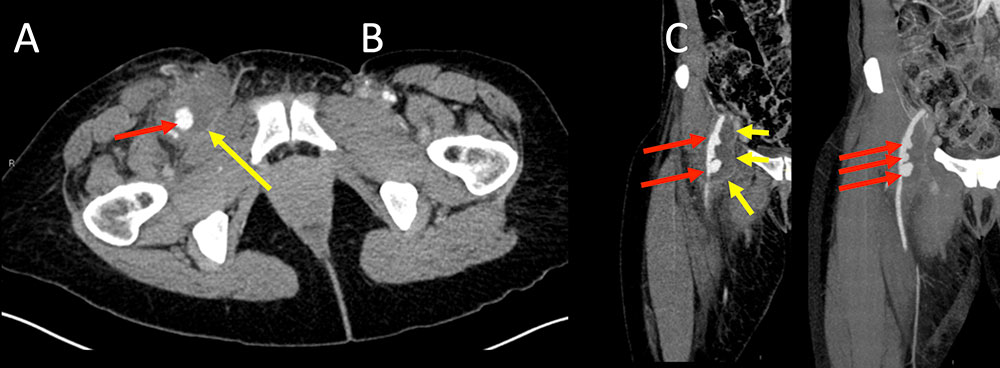 |
Vascular Complications Figure 9. 55 year old man with a 30 year history of intravenous drug use, HIV/AIDS, ESRD, presents with neck pain. IV contrast enhanced CT of the neck in axial plane (A) with coronal (B) and coronal maximal intensity projection (C) reconstructions. Impressive lobulated saccular 2.9 x 3.1 x 5.5 cm pseudoaneurysm (PSA) of the right common carotid artery secondary to intravenous drug injection. Broken needle tip (bottom A, B, C red short arrow) along the medial aspect of the PSA. Numerous other broken needle fragments present through the neck. Additional needle fragment within the right internal jugular vein (A, B, C gold arrow) which is partially thrombosed. 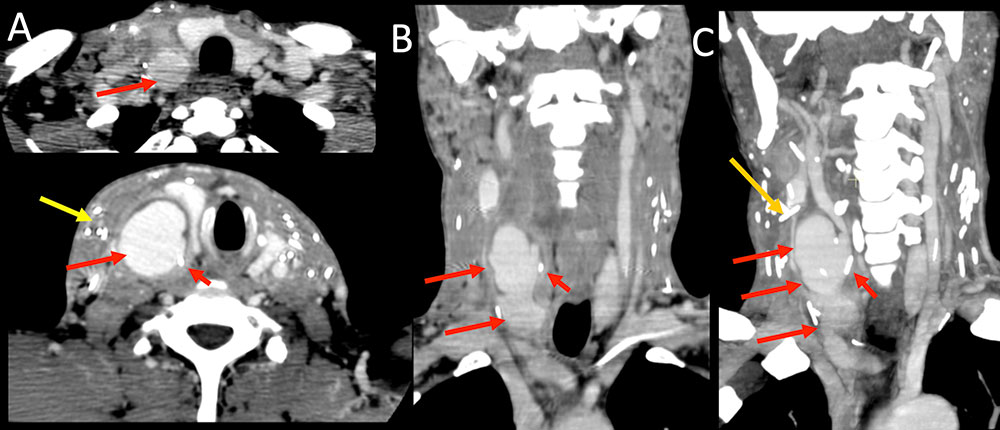 |
Retained Foreign Bodies
|
Retained Foreign Bodies Figure 10. 58 year old man with history of intravenous drug abuse (in remission 10 years) presents for chronic left hip pain evaluation. Frontal view of the pelvis and lateral view of the left hip demonstrates severe hip osteoarthritis. 2 well seen needle fragments are seen on both views (A, B, red arrows). Magnified view reveals a third fragment projecting over the femoral head (C, yellow arrow). 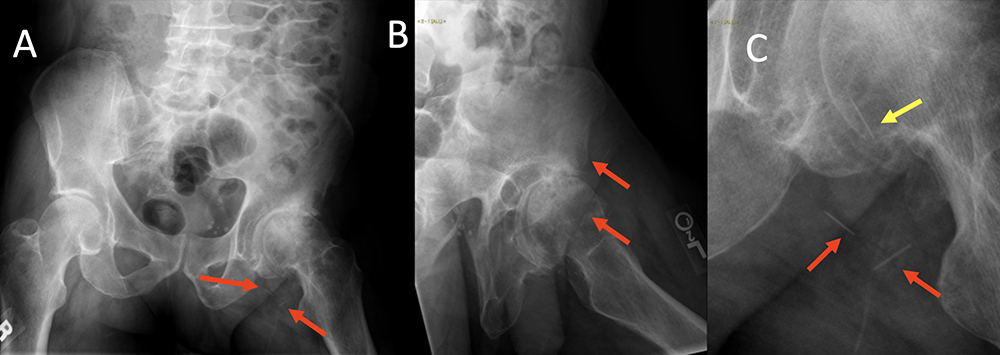 |
Retained Foreign Bodies Figure 11. 55 year old man with over 30 year history of intravenous drug use, HIV/AIDS, ESRD, presents with chest pain (same patient as in figure 9). Frontal chest radiograph magnified to the supraclavicular regions demonstrates scattered needle fragments (A, red arrows). There is markedly improved visualization of the number of retained needles with edge enhancement filter available in standard PACS viewer (B, red circles). A tunnel hemodialysis catheter and sternotomy wires are partially visualized. 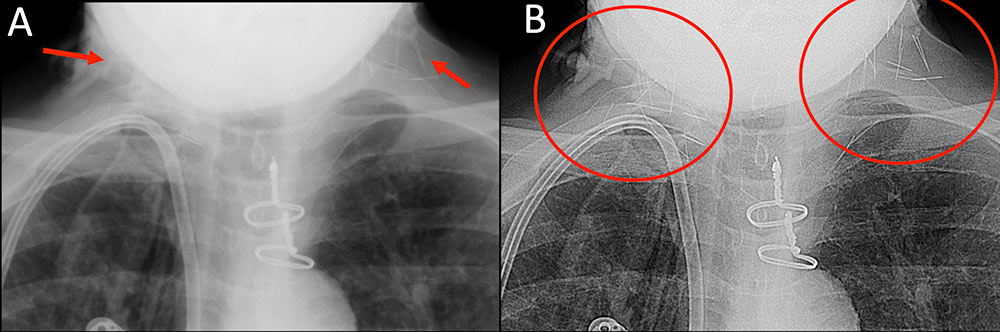 |
Retained Foreign Bodies Figure 12. 31 year old woman unknown duration of intravenous drug abuse presented to the ED in police custody with recurrent bacteremia with treatment for renal abscess. IV contrast enhanced axial CT image of the pelvis (A) with oblique coronal reconstructions (B and C) demonstrates 4 air filled tubular structures in the vagina (A, read and yellow arrows). Three structures are the same (A, red arrows) with a larger diameter structure to the left (A, yellow arrow). Only with interactive multiplanar reconstructions are the foreign bodies well visualized as small bore syringes (red arrows) and a vial (yellow arrow). One syringe has an uncapped bent needle (B, red arrow) with the adjacent cap (B, red arrowhead). A fully capped needle is well seen (C, red arrow). The patient apparently panicked and inserted her drug paraphernalia into her vagina prior to police custody. 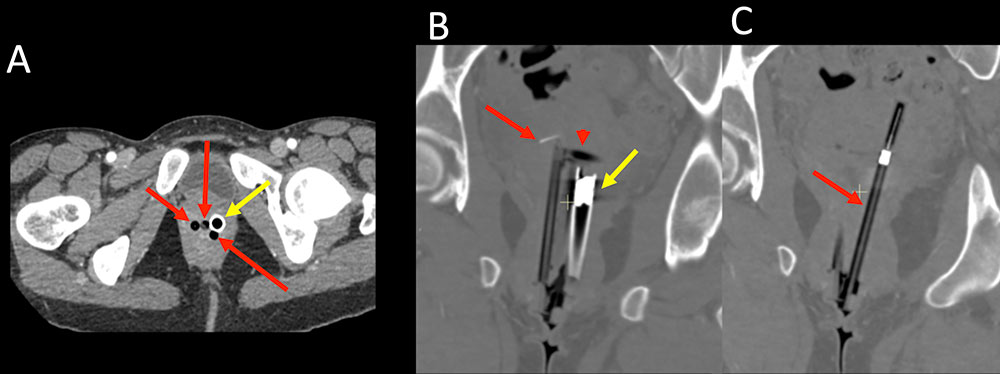 |
Embolic Complications
|
Embolic Complications
|
Embolic Complications Figure 13. 45 year old woman with active polysubstance abuse including injecting intravenous heroin presents with difficultly walking and hip pain. Non-contrast CT of the pelvis in axial (A) and coronal (B) planes demonstrates destruction of the pubic symphysis compatible with osteomyelitis (A, B red arrows). MRSA was cultured directly from pubic symphysis bone biopsy and from blood cultures. 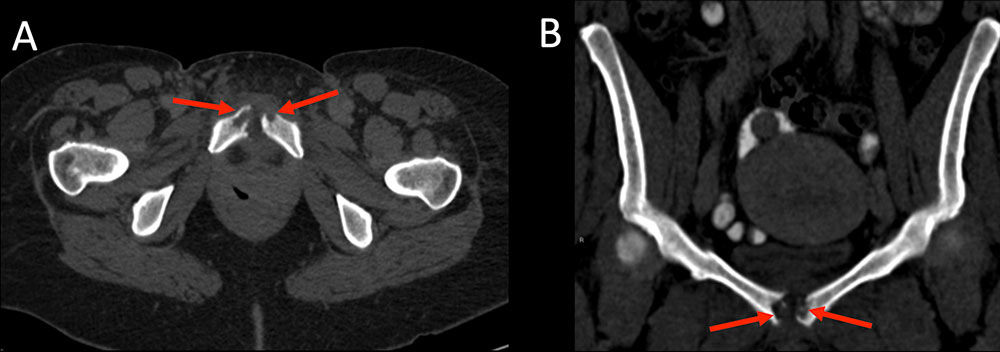 |
Embolic Complications Figure 14. 31 year old woman with active intravenous drug abuse presents with one week of fever. Non-contrast CT of the chest in axial (A, B), and coronal (C) planes demonstrates multiple solid nodules, some cavitary, predominately throughout the lower lobes with a few nodules in the upper lobes (red arrows). Note the ill-defined margins of the nodules with subtle hazy ground glass opacity. Nodules are consistent with septic emboli. Blood cultures were positive for methicillin-susceptible Staphylococcus aureus (MSSA). 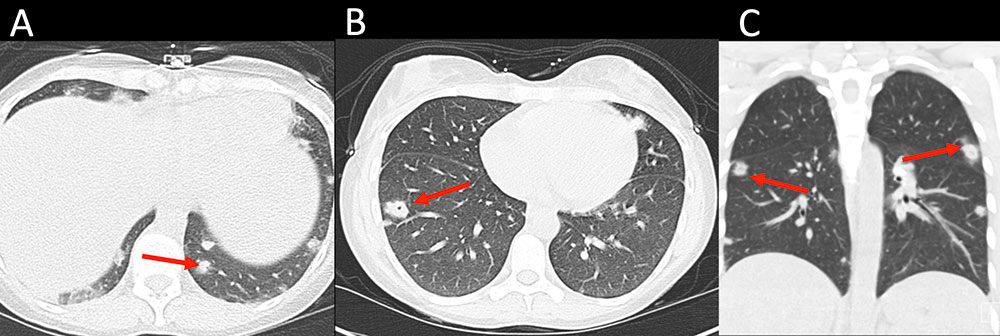 |
Conclusions
|
References
|
References
|
References
|
References
Acknowledgements
|
