The Role Of Cinematic Rendering In The Detection And Evaluation Of Suspected Hepatic Tumors: How We Do It
The Role Of Cinematic Rendering In The Detection And Evaluation Of Suspected Hepatic Tumors: How We Do It Elliot K. Fishman MD Linda Chu MD Satomi Kawamoto MD Johns Hopkins Hospital |
The role of 3D imaging in the liver has classically focused on a combination of classic volume rendering (VRT) and maximum intensity projection (MPR) techniques. While the literature has shown a range of clinical applications for 3D imaging ranging from pre-operative planning for hepatic resection, to vascular mapping for lesion definition and pattern recognition, to detection of vascular complications (arterial and venous) the introduction of cinematic rendering has to date not seen universal adoption as a valuable adjunct especially for liver tumors. In this exhibit we will try to define our experience with cinematic rendering (CR) in the evaluation of the liver focusing on the evaluation of hepatic masses. Discussion into the realm of vascular evaluation in cirrhosis (i.e. vascular malformation or shunting) or the patient post trauma (i.e. bleeding from the hepatic artery)or post liver transplant (i.e. hepatic artery patency) is beyond the scope of this exhibit. |
Cinematic Rendering of Liver: Protocol and Technical Notes
|
Our experience with Cinematic Rendering of the Liver is also Referring Physician Driven
|
Hepatoma: MIP vs Cinematic Rendering with CR Texture Mapping 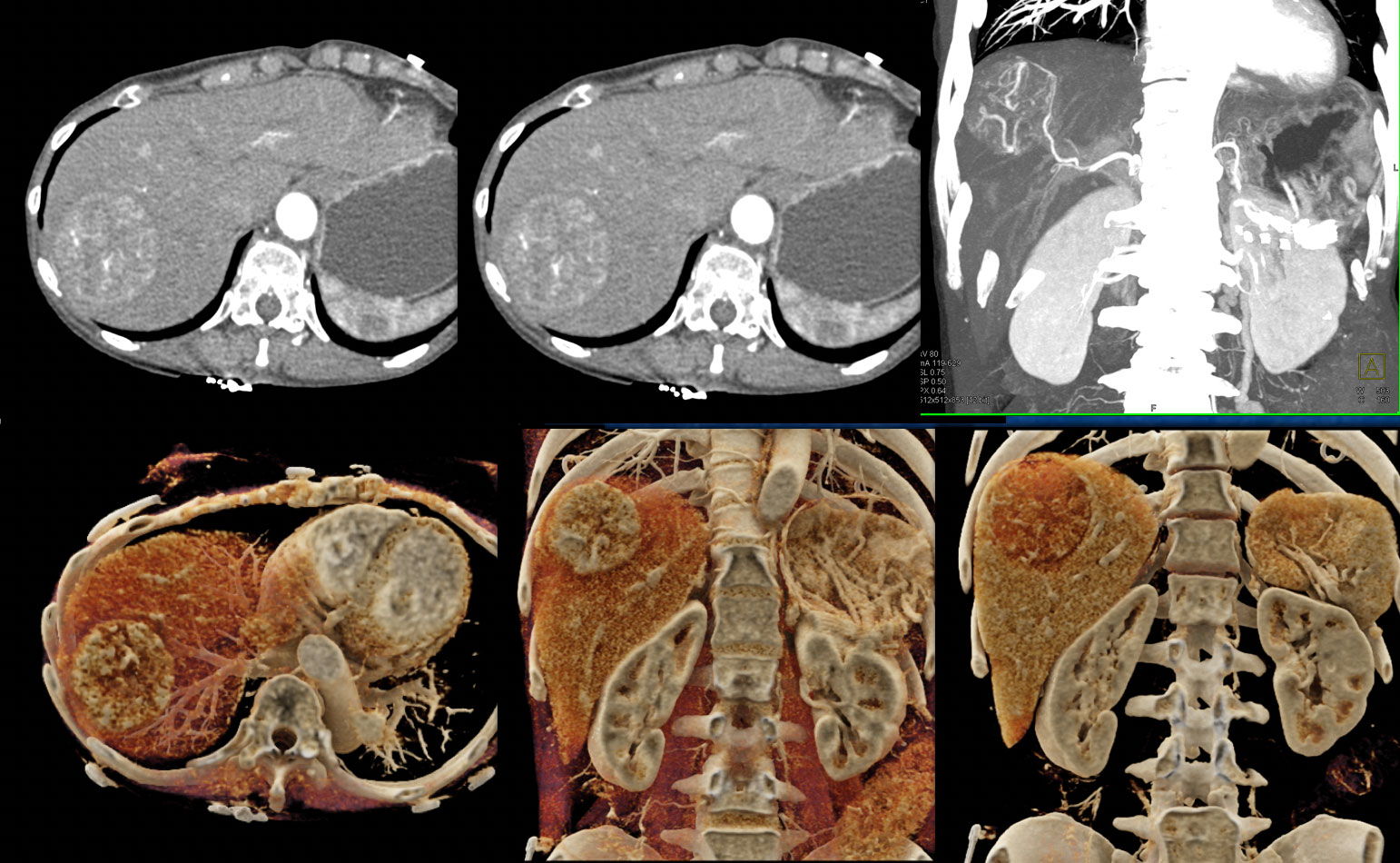 |
Hepatoma in Cirrhotic Liver Comparing VRT, MIP and CR 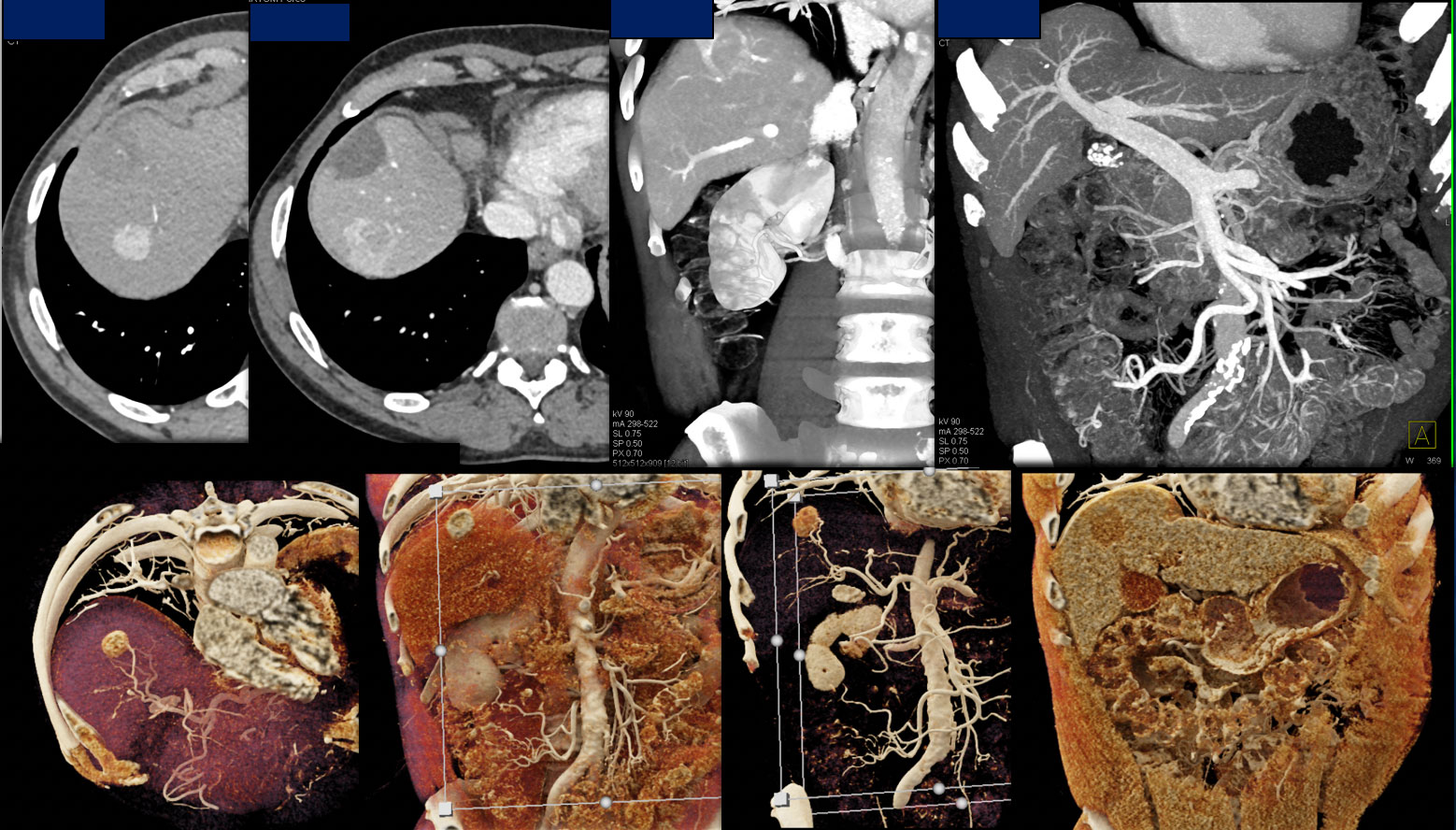 |
Cinematic Rendering of the Liver: Applications
|
Benign Hepatic Tumors Cinematic Rendering helps define many of the classic signs of various benign tumors including hemangioma, focal nodular hyperplasia (FNH), and hepatic adenoma (HA). The CR images nicely define the vascular map and the cases show the pattern of lesions with CR and compare it to dual phase imaging and classic VRT and MIP reconstruction. |
Vascular mapping of the liver mass in a pattern classic for hemangioma 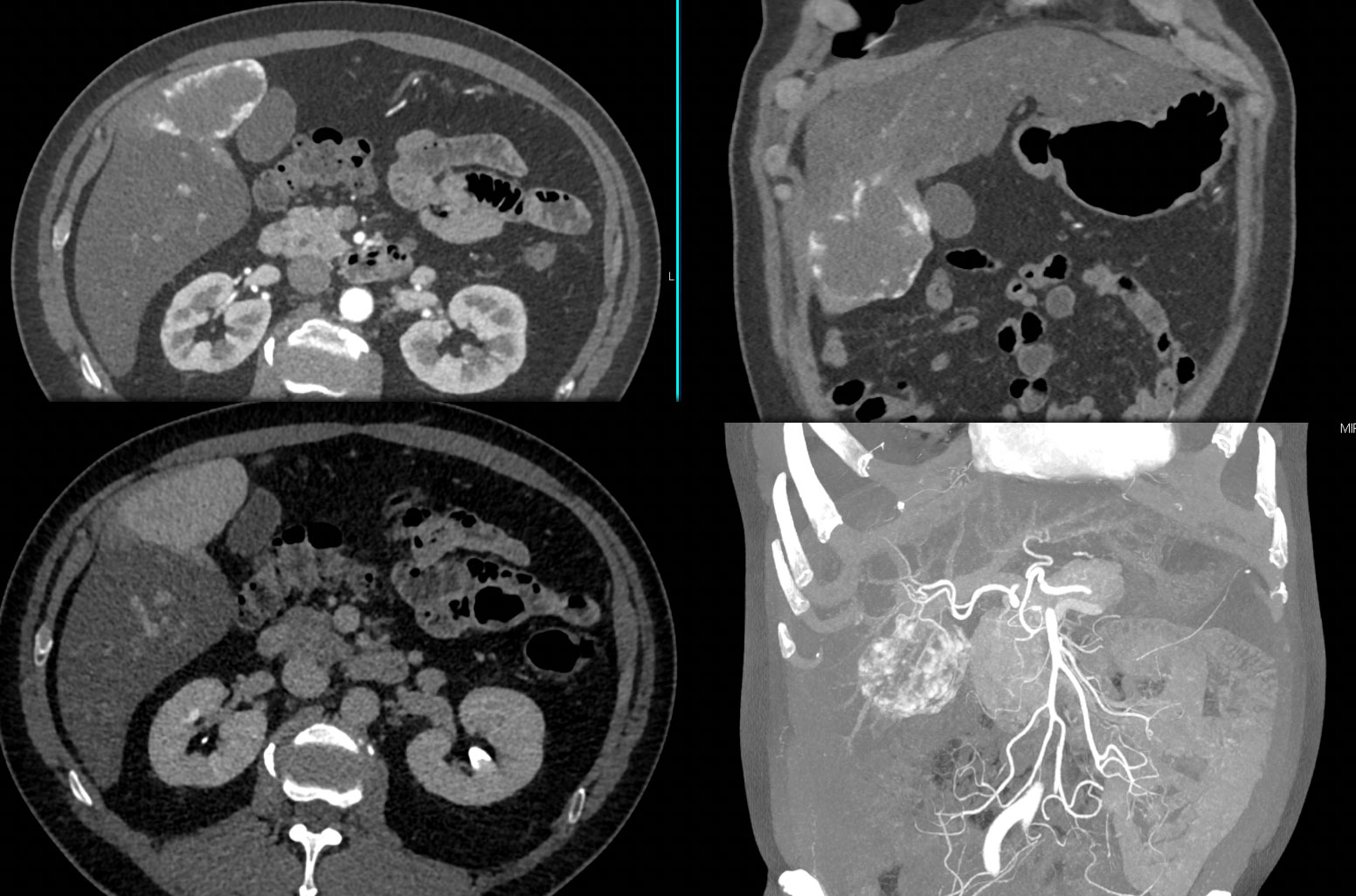 |
Range of CR images using a number of presets of a hepatic hemangioma. 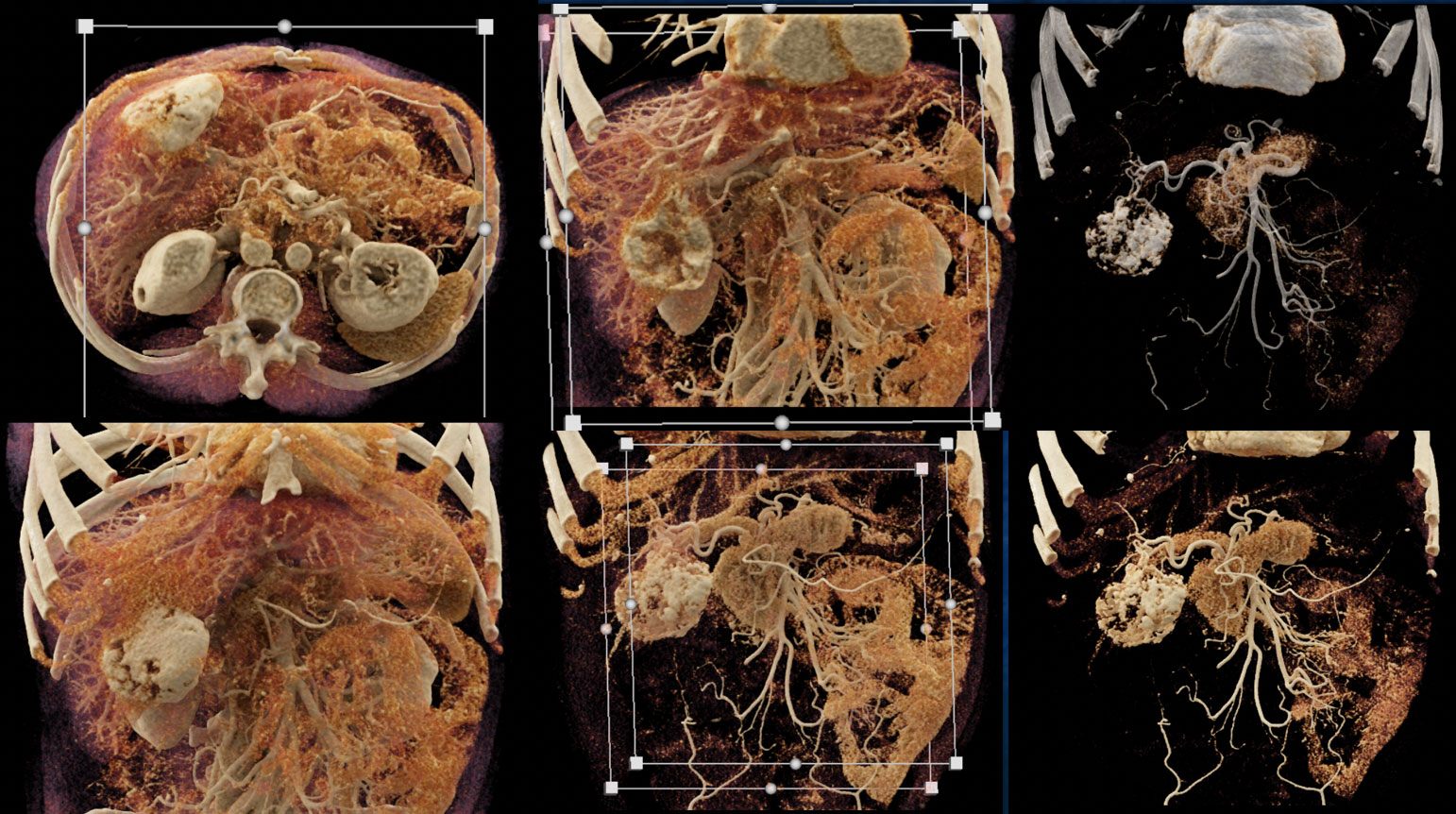 |
Incidental FNH with classic enhancement similar to the IVC on arterial images and the lesion becomes isodense on venous phase imaging. 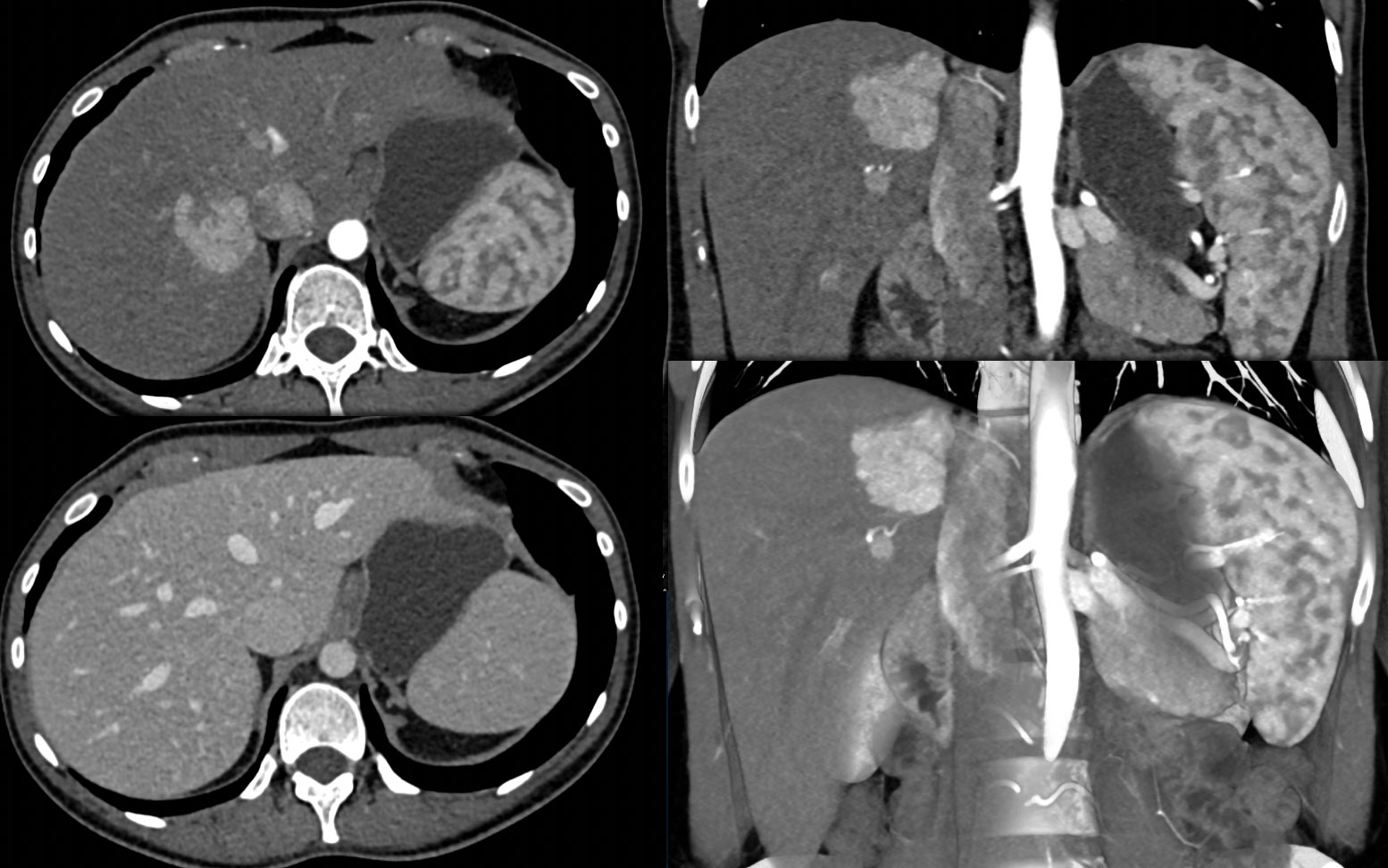 |
 |
Vascular enhancement on arterial phase imaging which becomes isodense on venous phase imaging classic for Hepatic Adenoma. 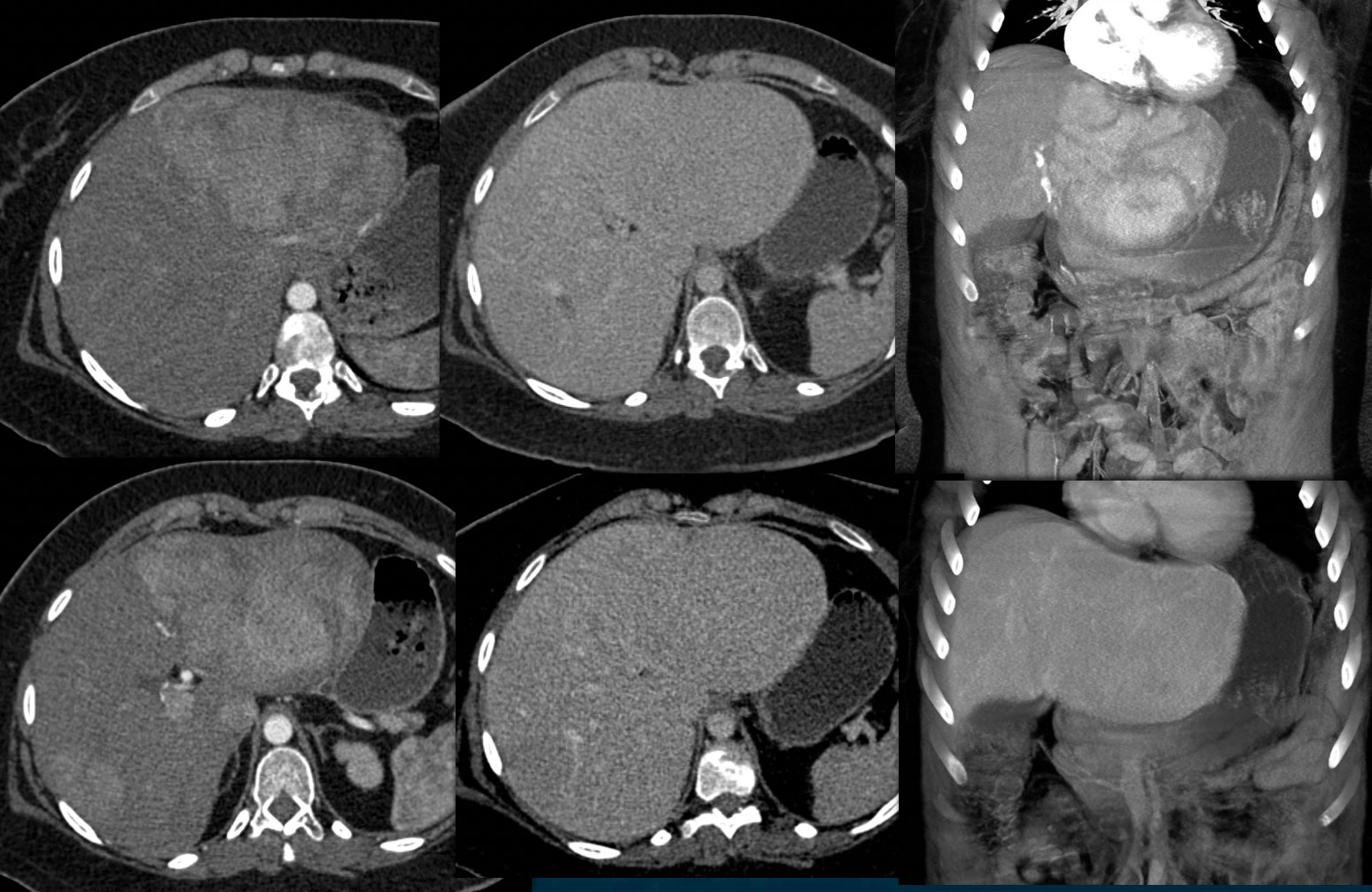 |
 |
Multiple lesions under 1cm are multifocal hepatic adenomas. 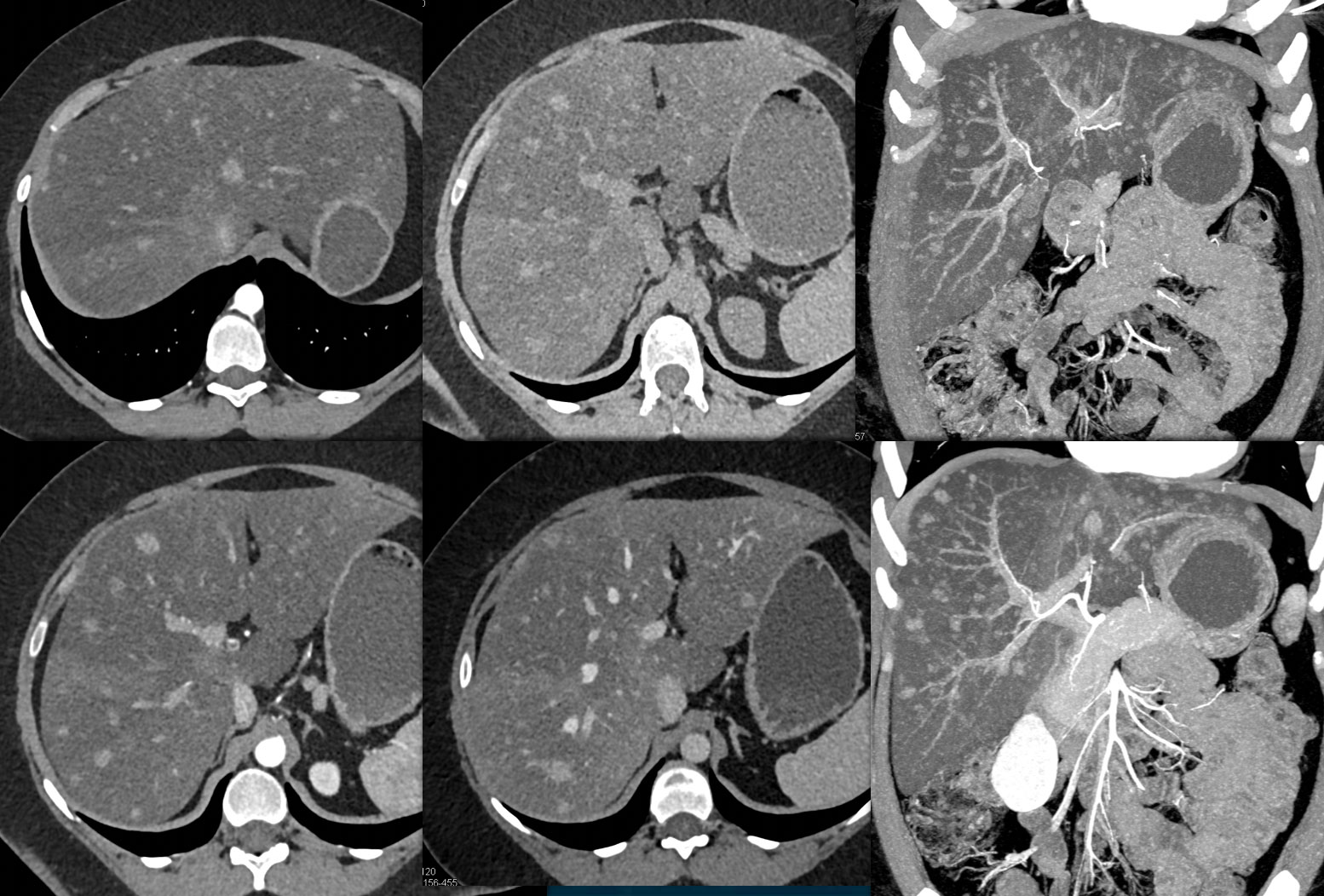 |
Multiple hepatic adenomas under 5 mm in size seen in the liver on CR. 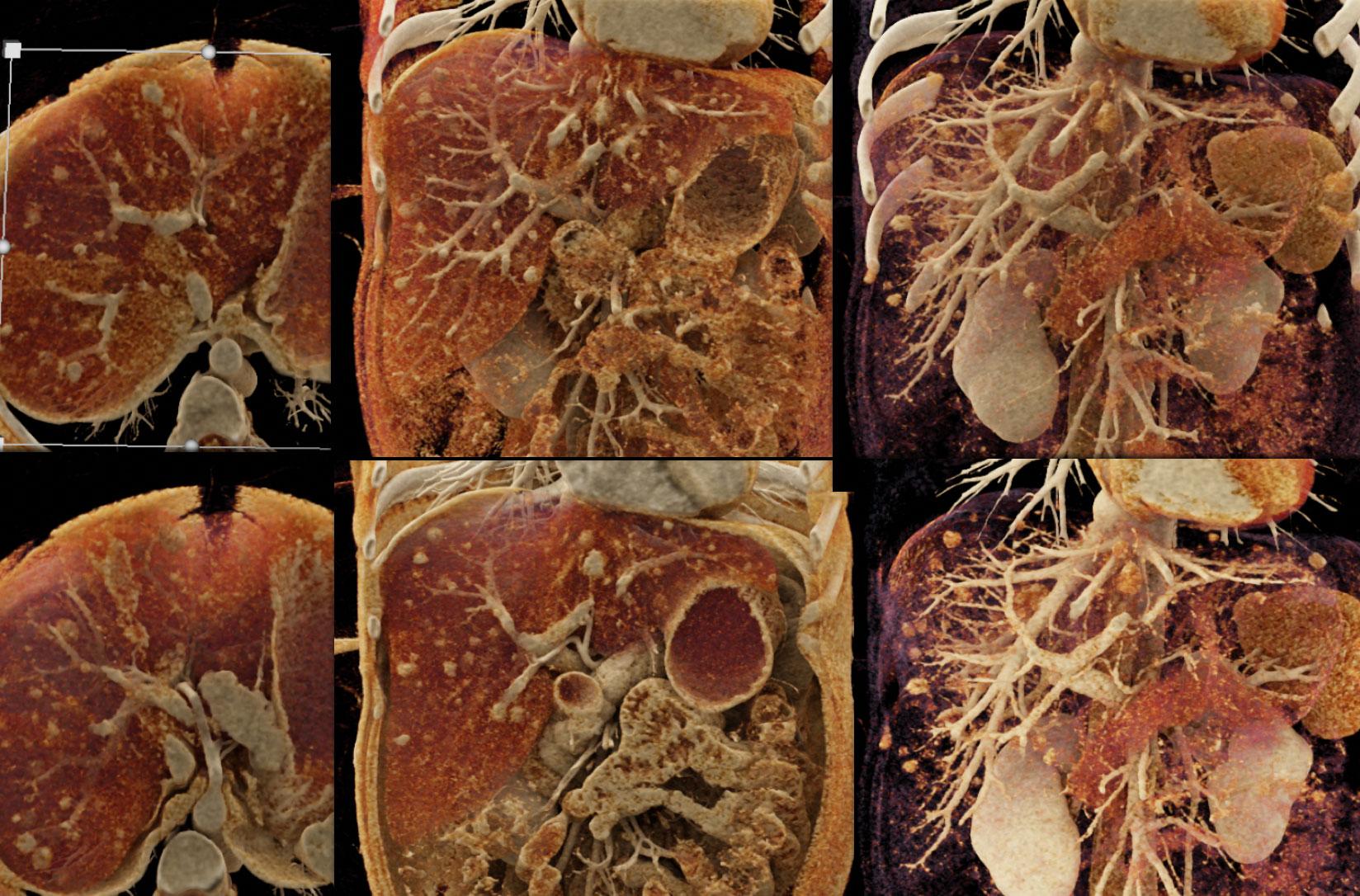 |
CTA in arterial and venous phase imaging with the lesion seen best on on venous phase imaging. This is one of the patterns for Hepatoma. 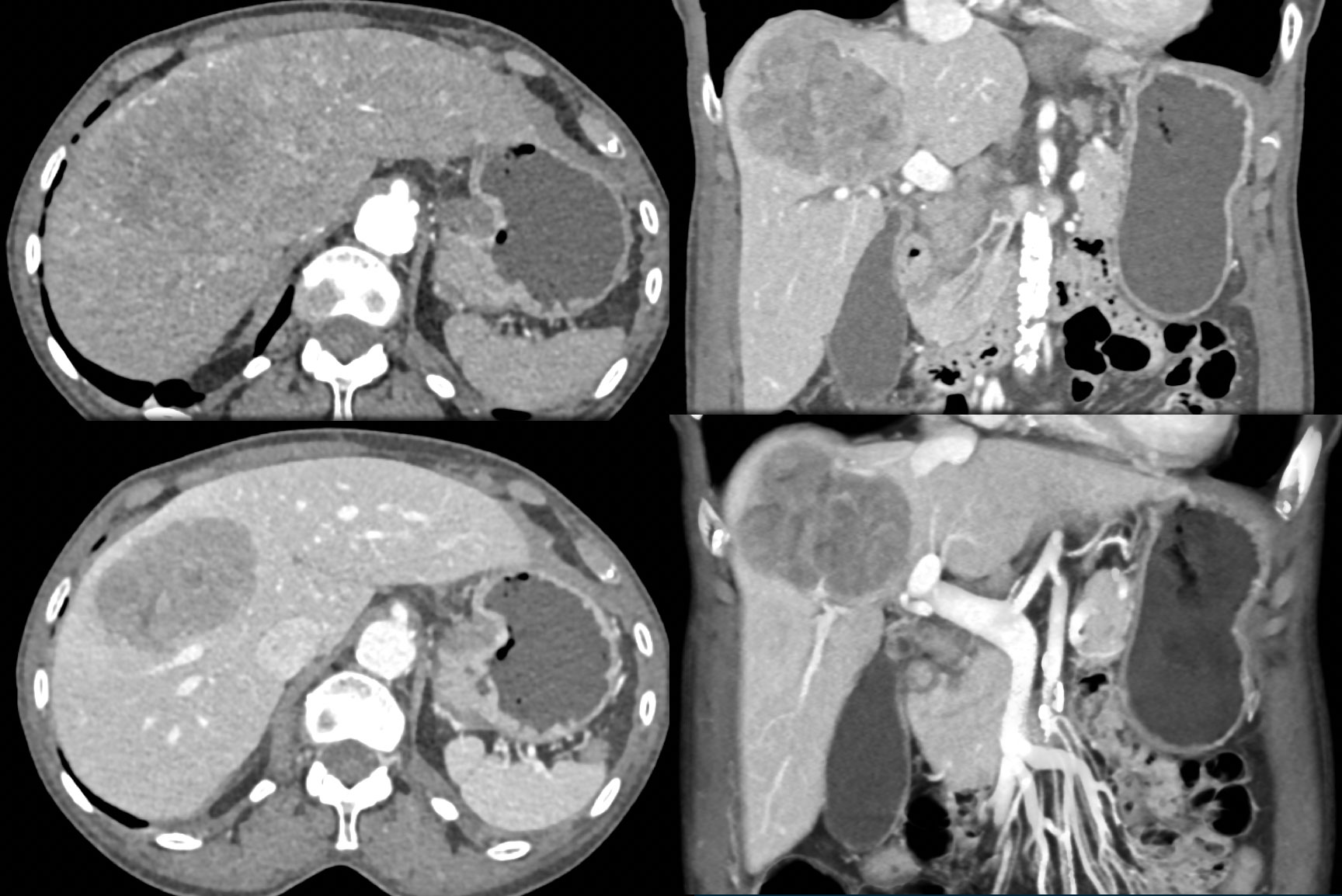 |
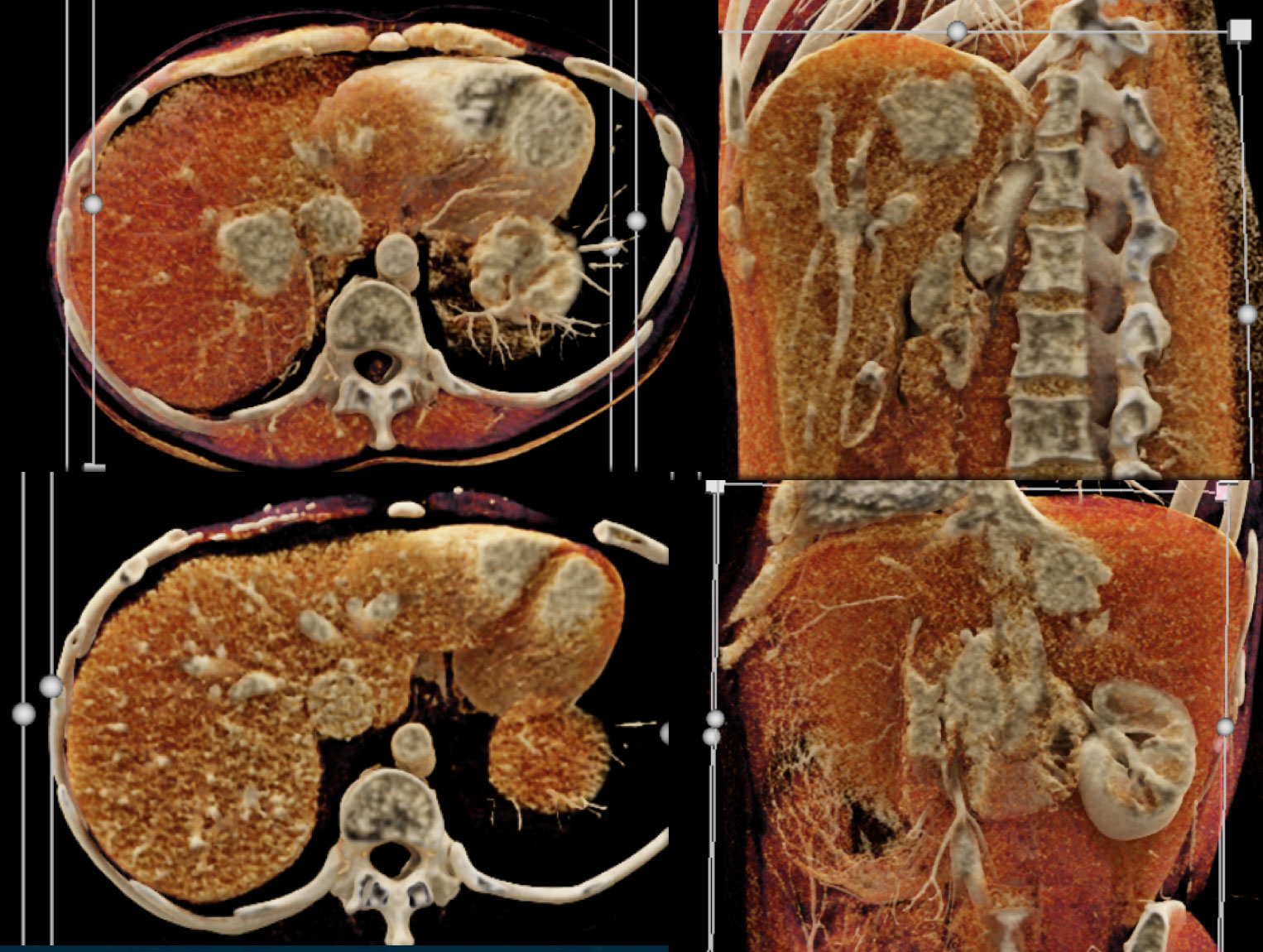
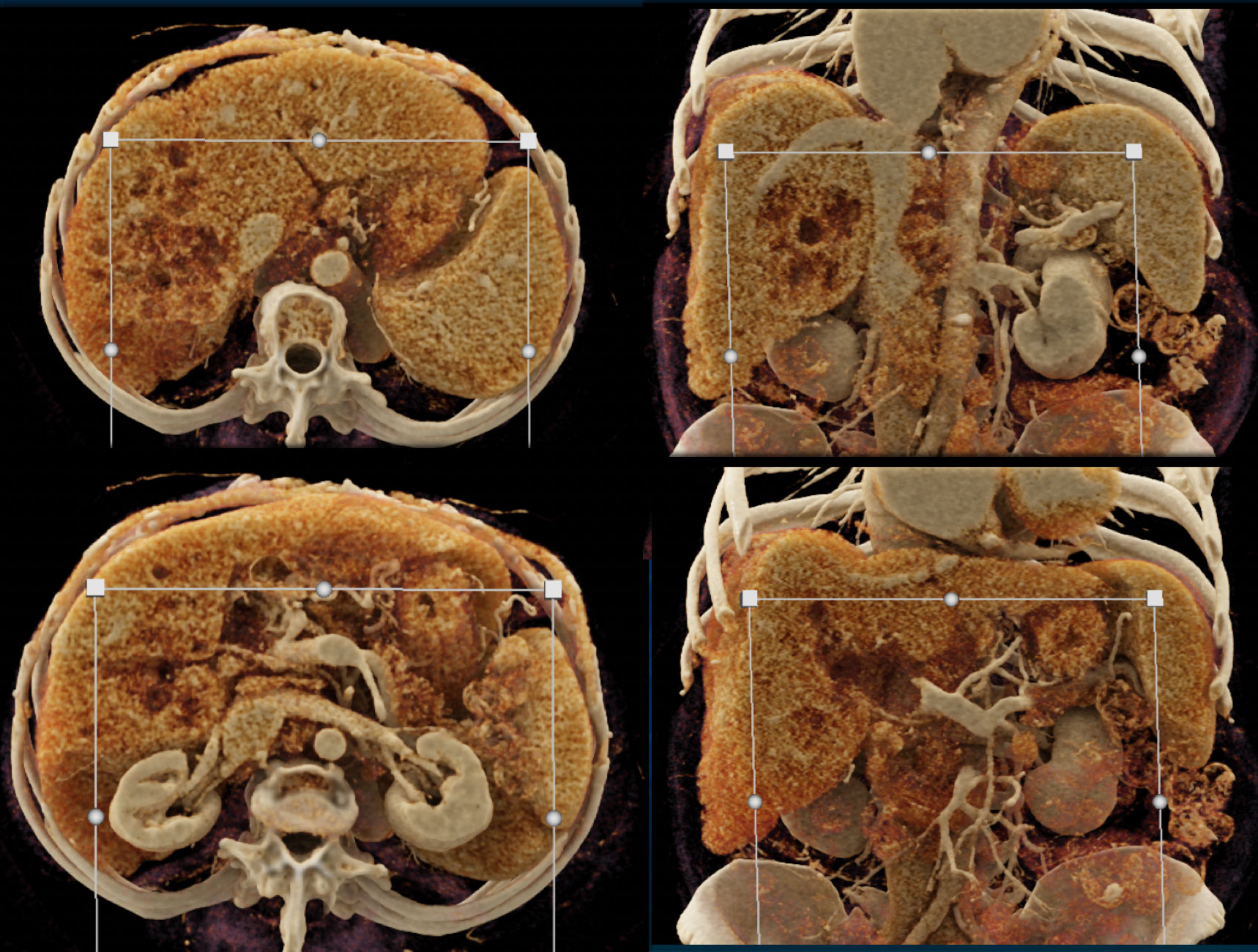
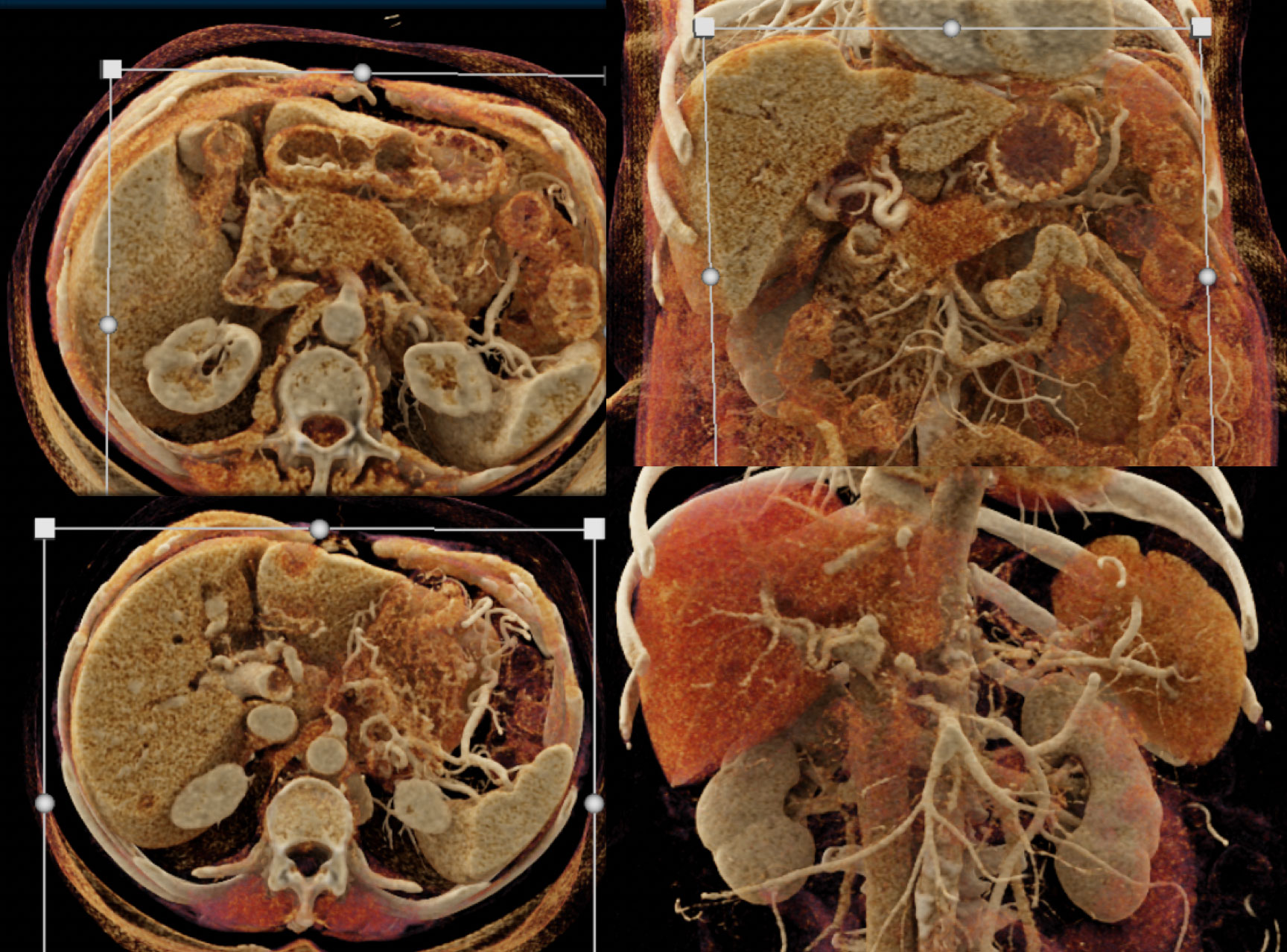
Range of Cinematic Rendering Appearances of the Hepatoma. 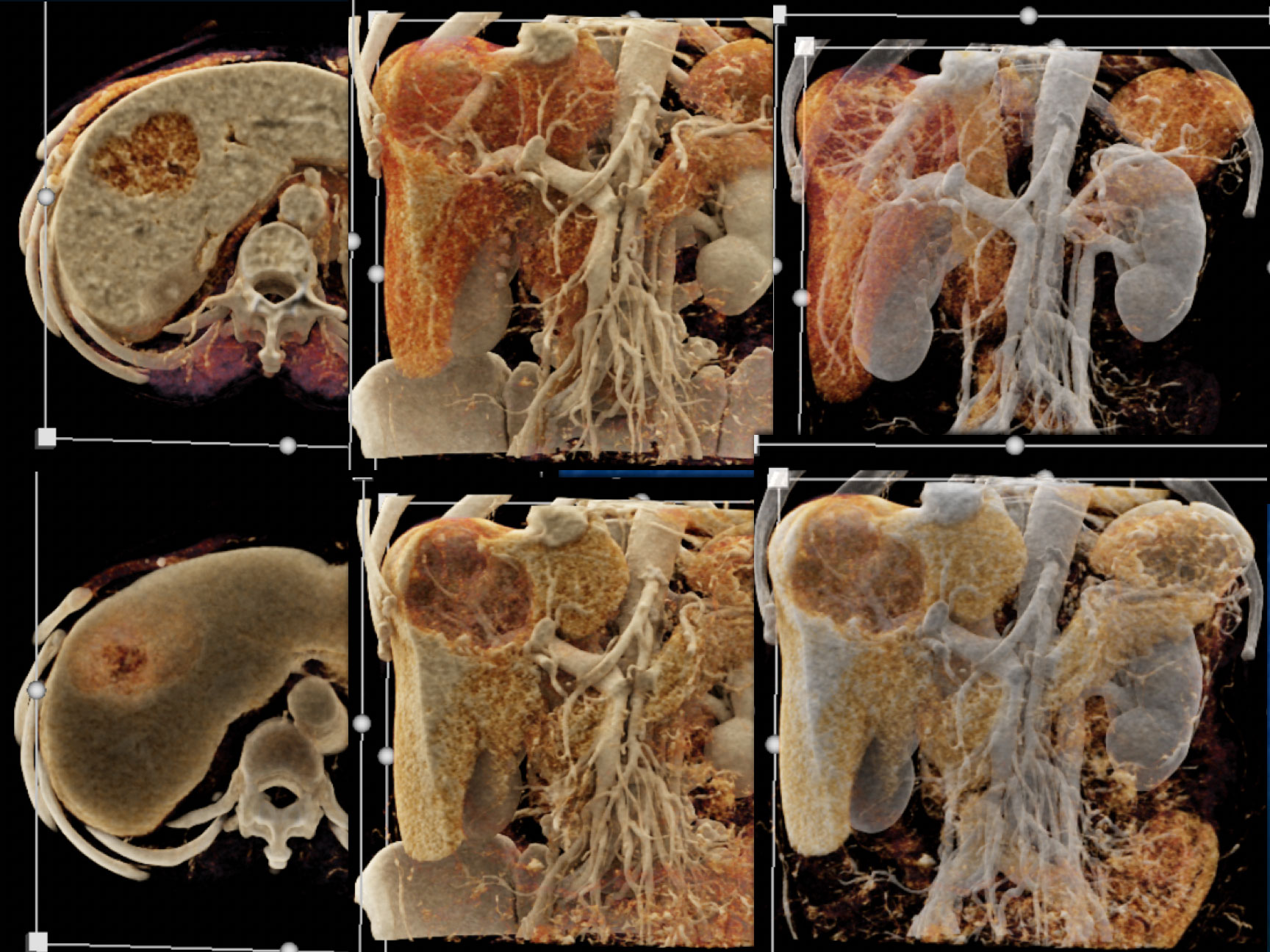 |
CTA of Hepatoma which is hypovascular in the left lobe of the liver. The CR images nicely define the mass for pre-op planning. 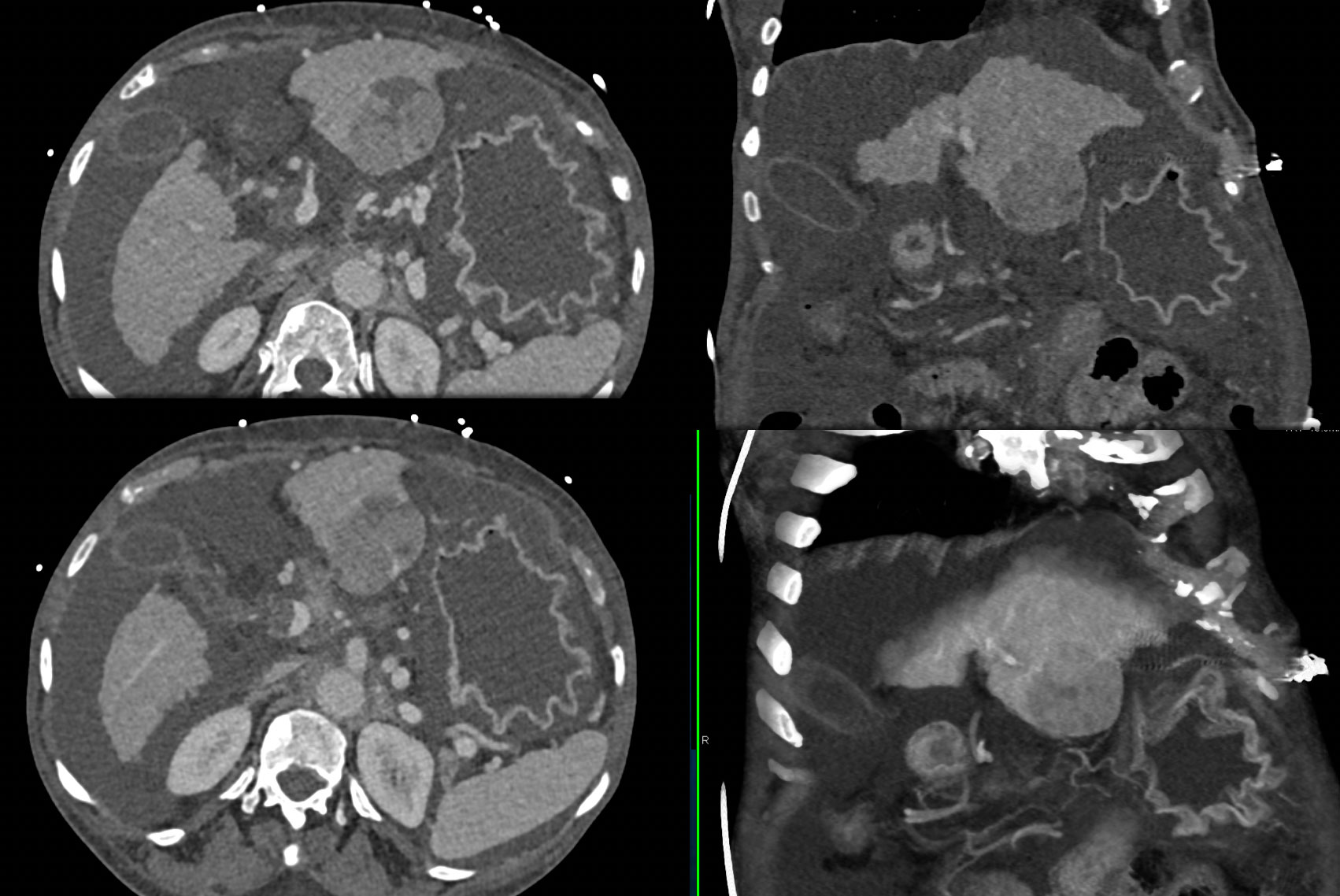 |
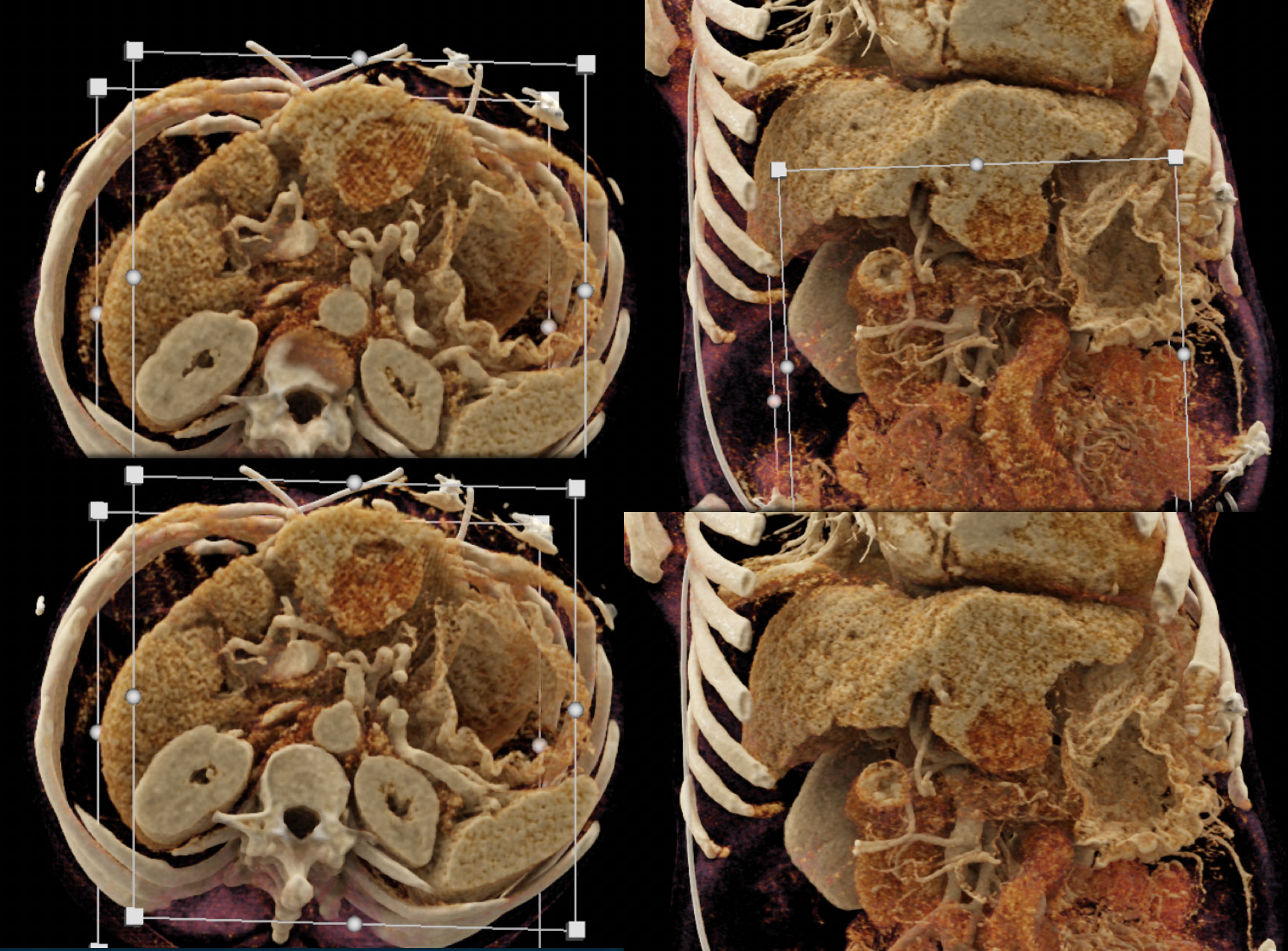 |
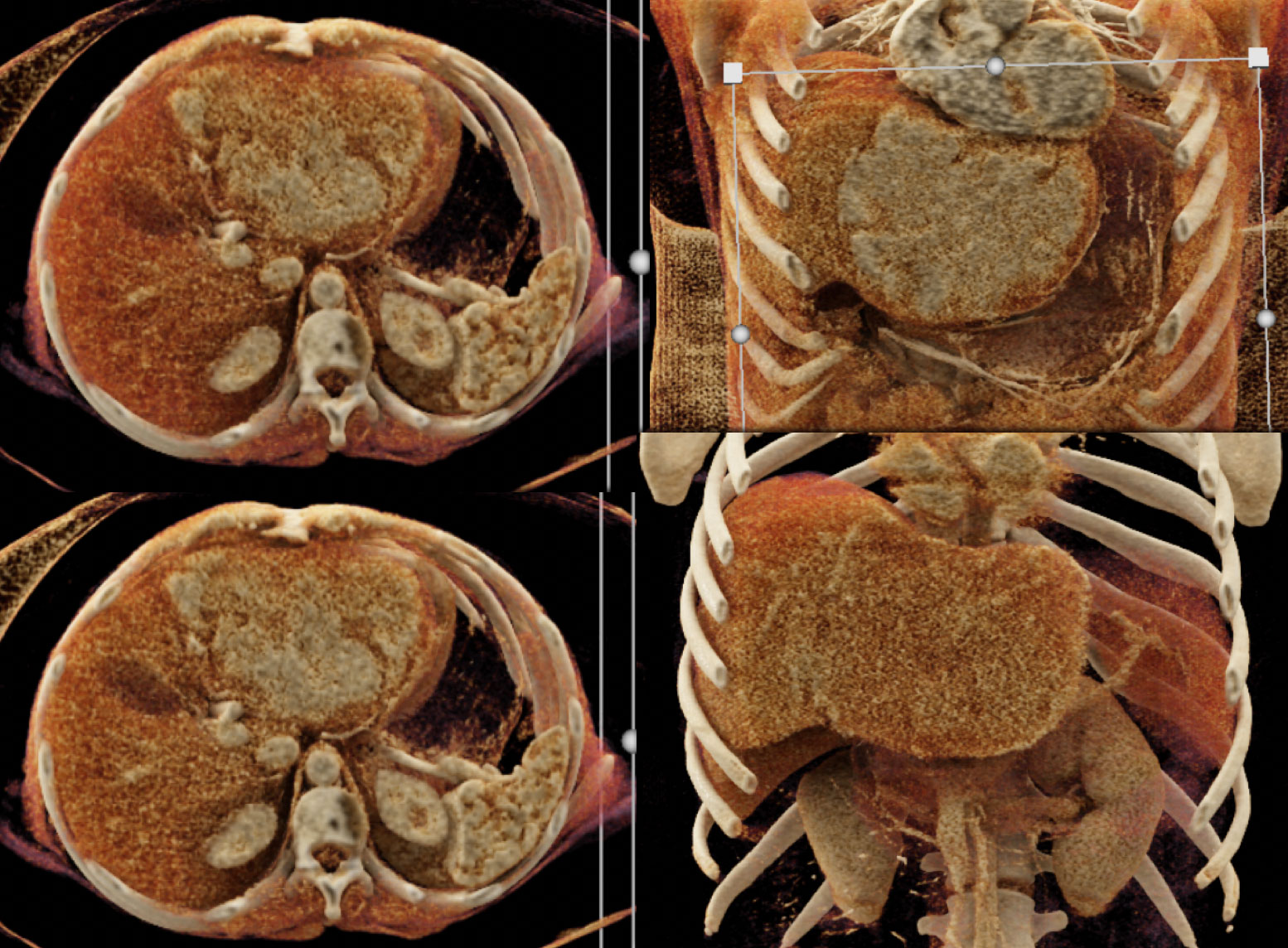
Fibrolamellar HCC in a young female 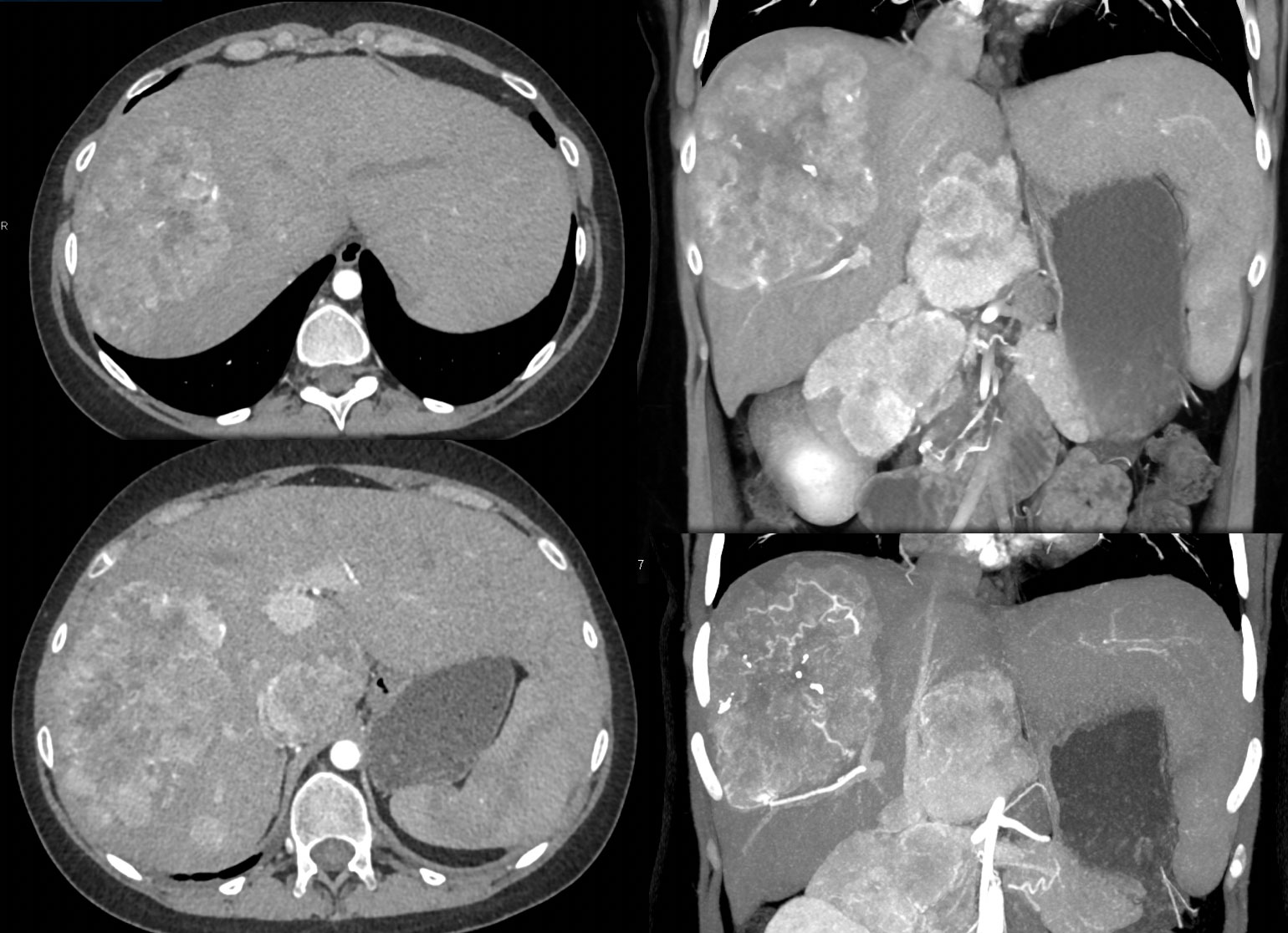 |
CR demonstrates the large mass with neovascularity. Bulky adenopathy is also seen. 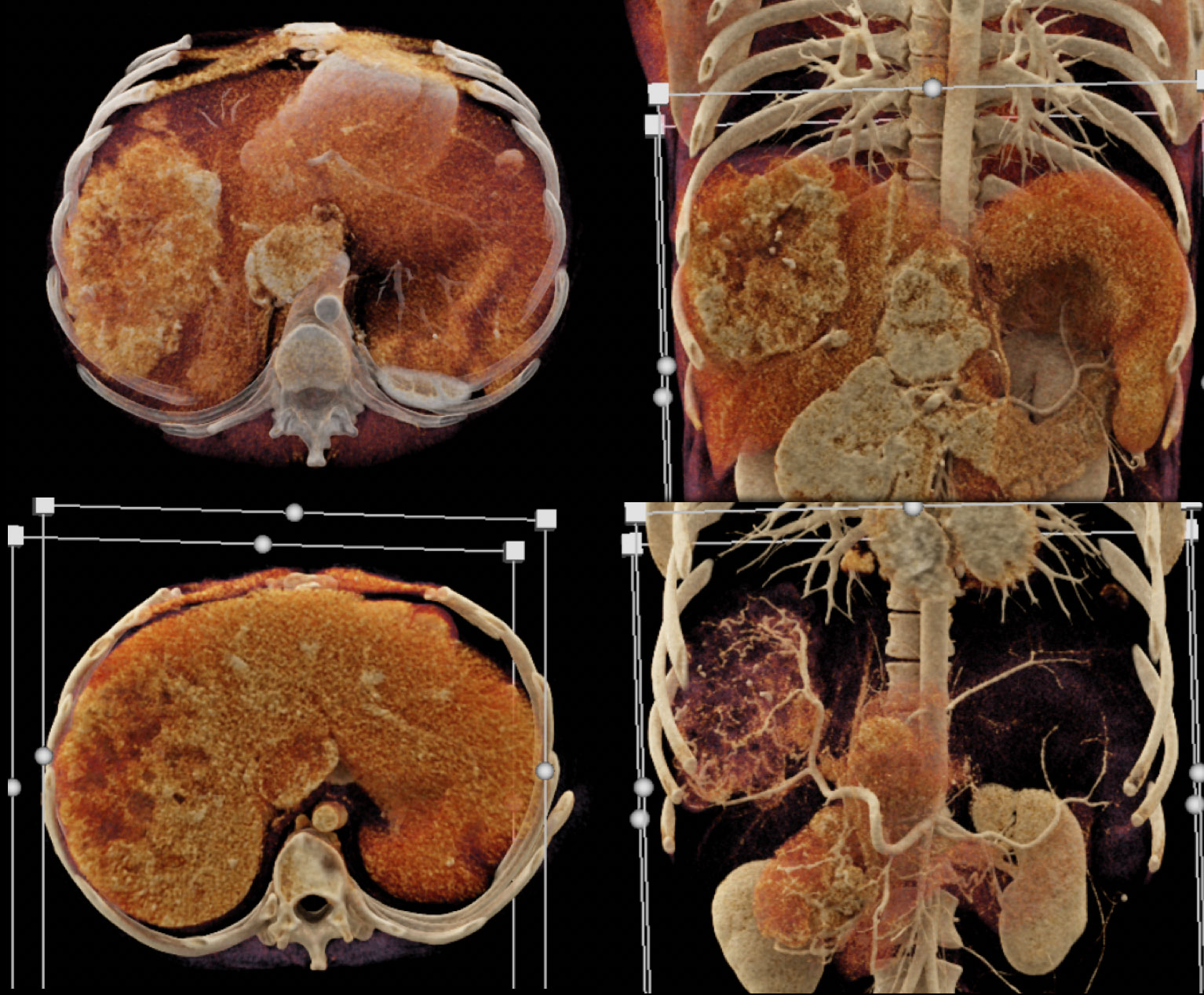 |
Intrahepatic Cholangiocarcinoma shows rim enhancement with no significant vascularity 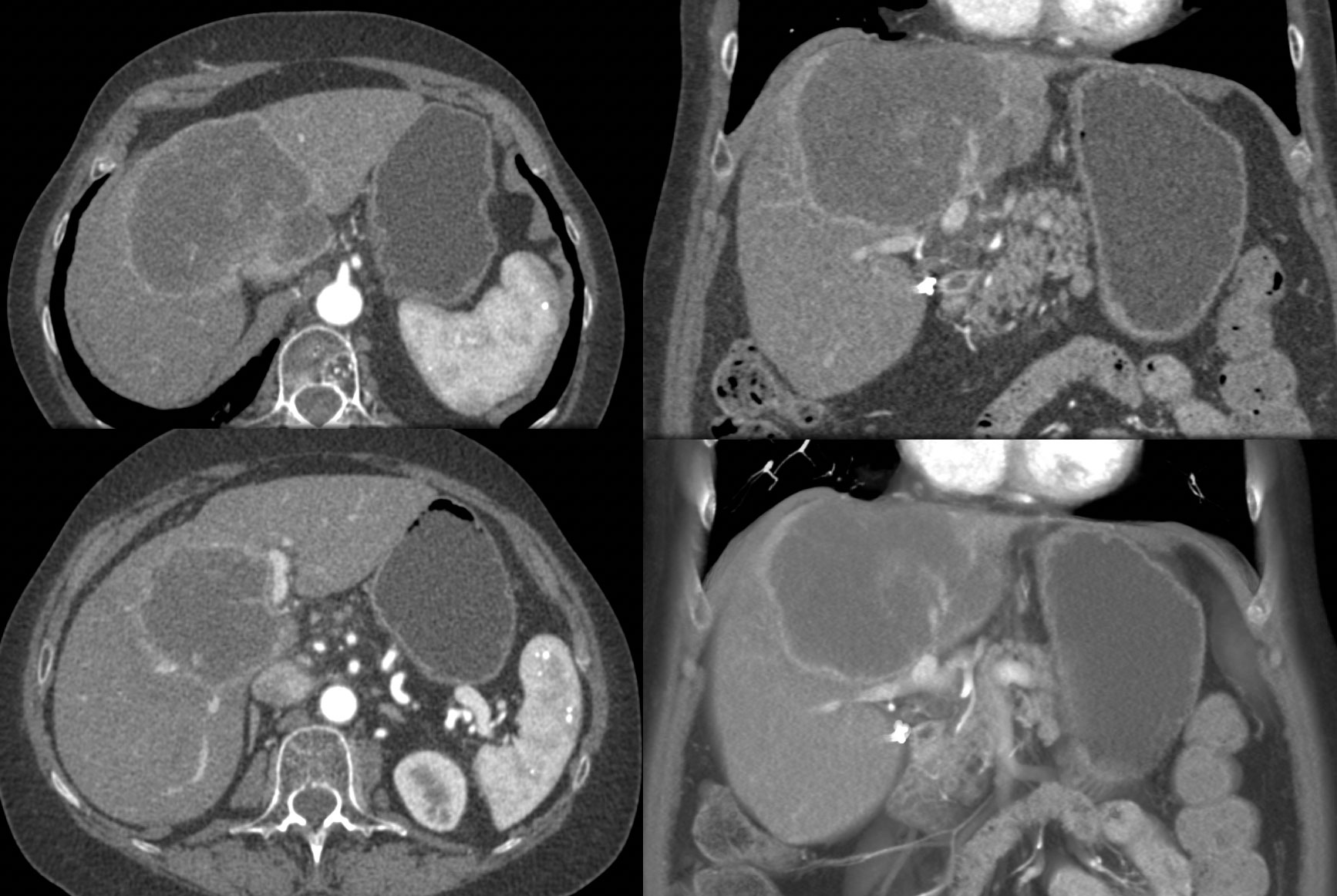 |
The CR nicely defines the pseudocapsule of the tumor with enhancement of the tumor wall. 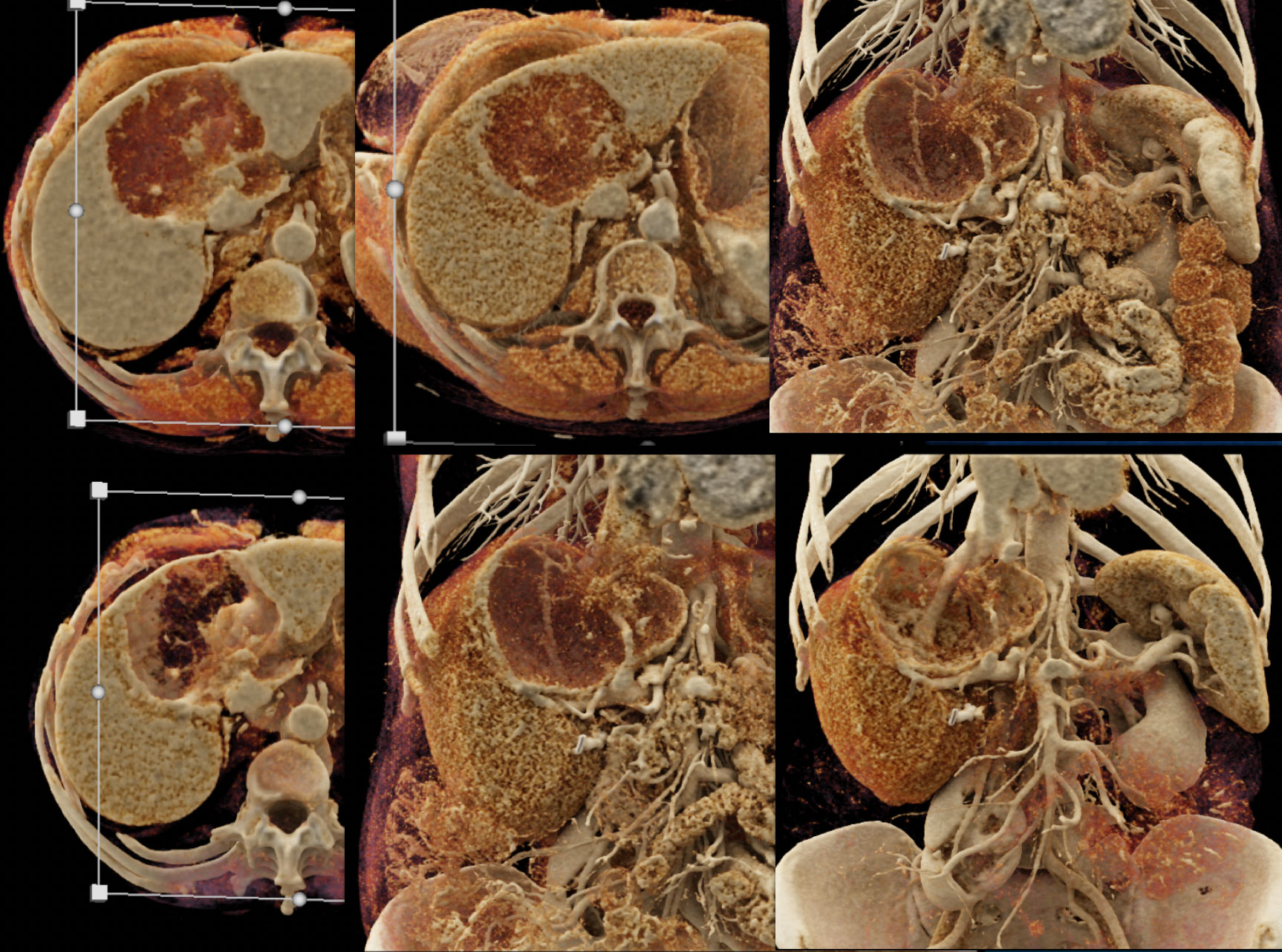 |
Cholangiocarcinoma with neovascularity looks similar to HCC with portal vein extension. MIP best defines the neovascularity 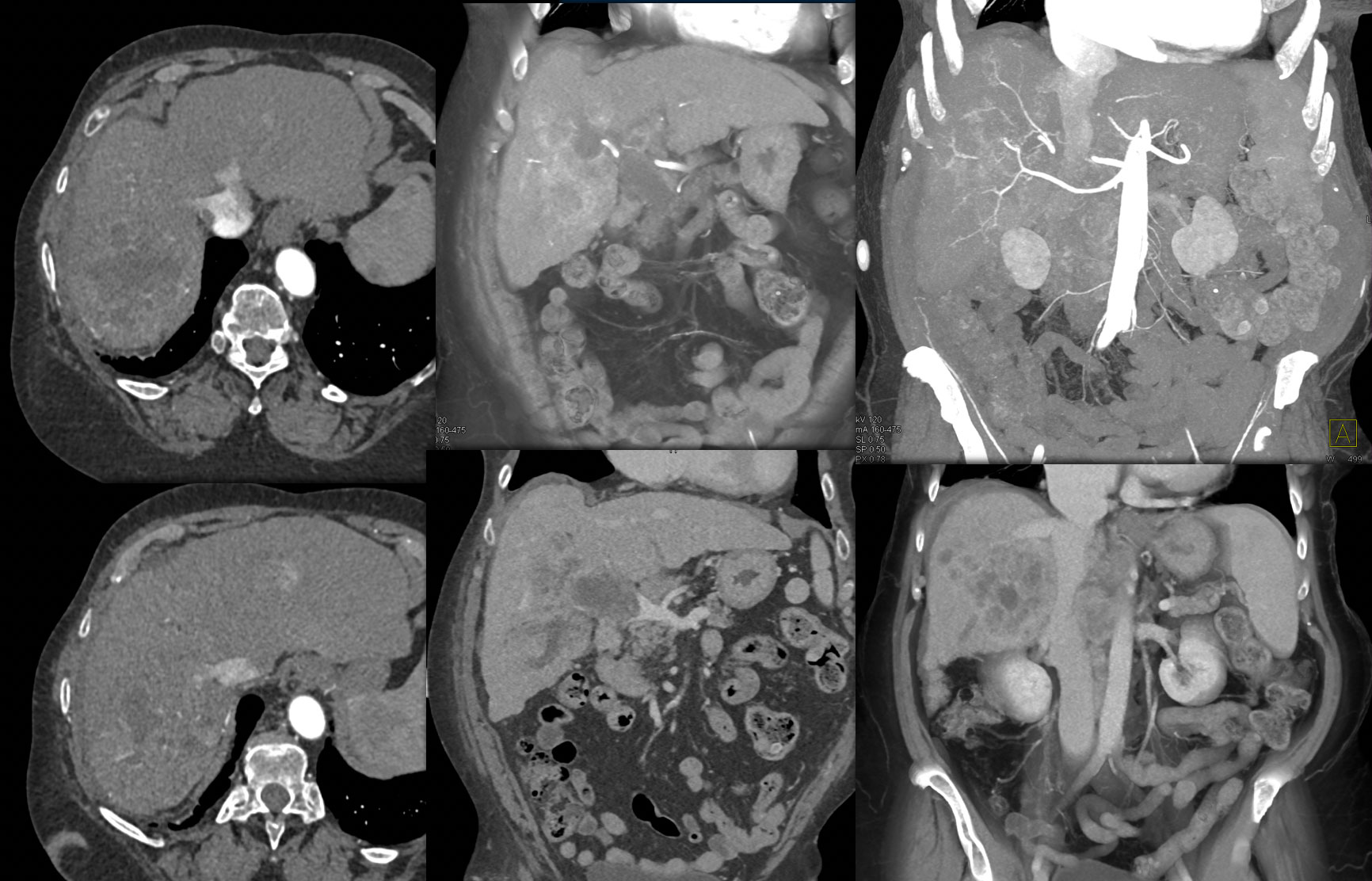 |
 |
Adenocarcinoma Body of the Pancreas with liver metastases that are hypovascular metastases. 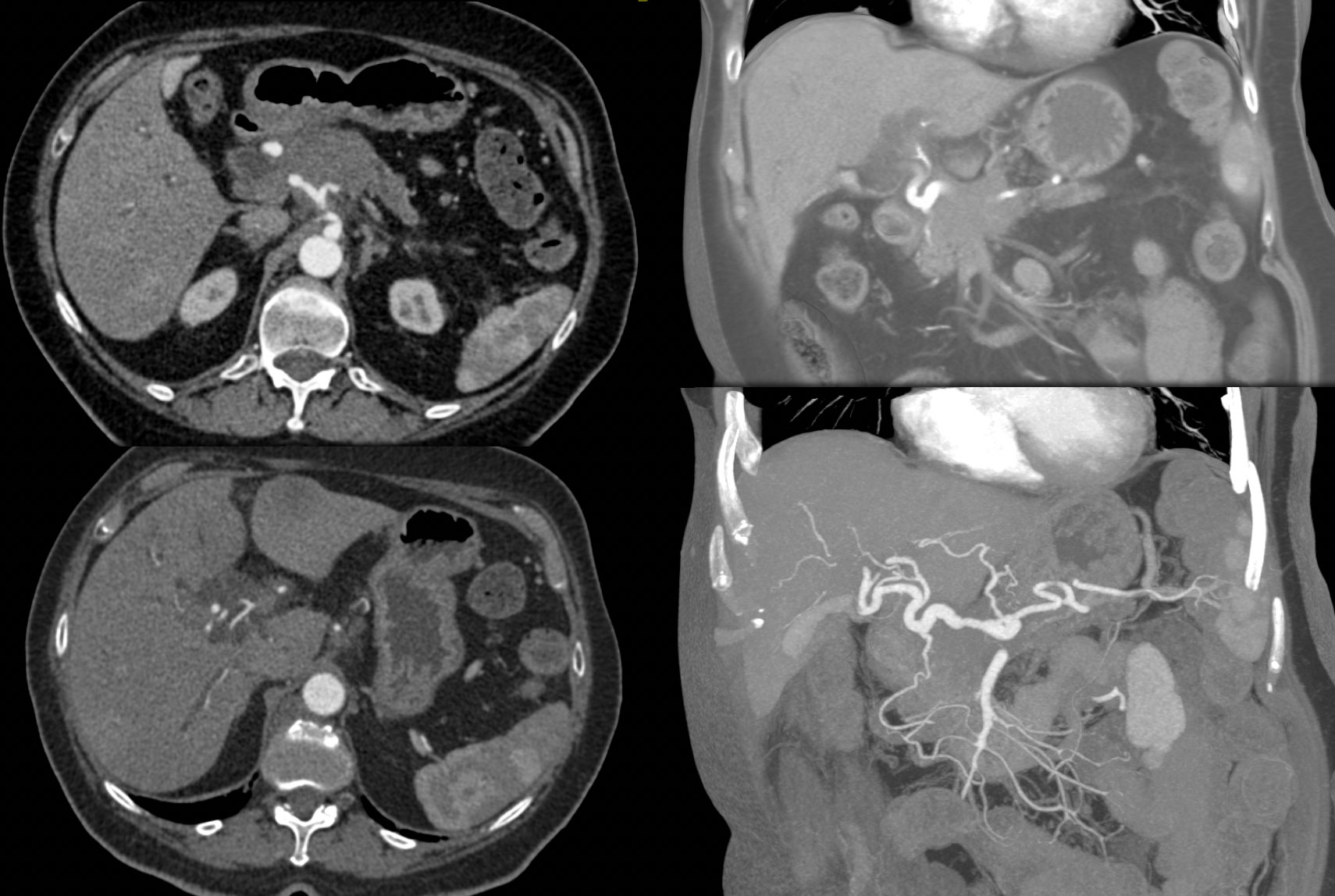 |
 |
Duodenal Carcinoid Tumor with liver metastases that are hypervascular.  |
Vascular metastases best seen on select CR images. 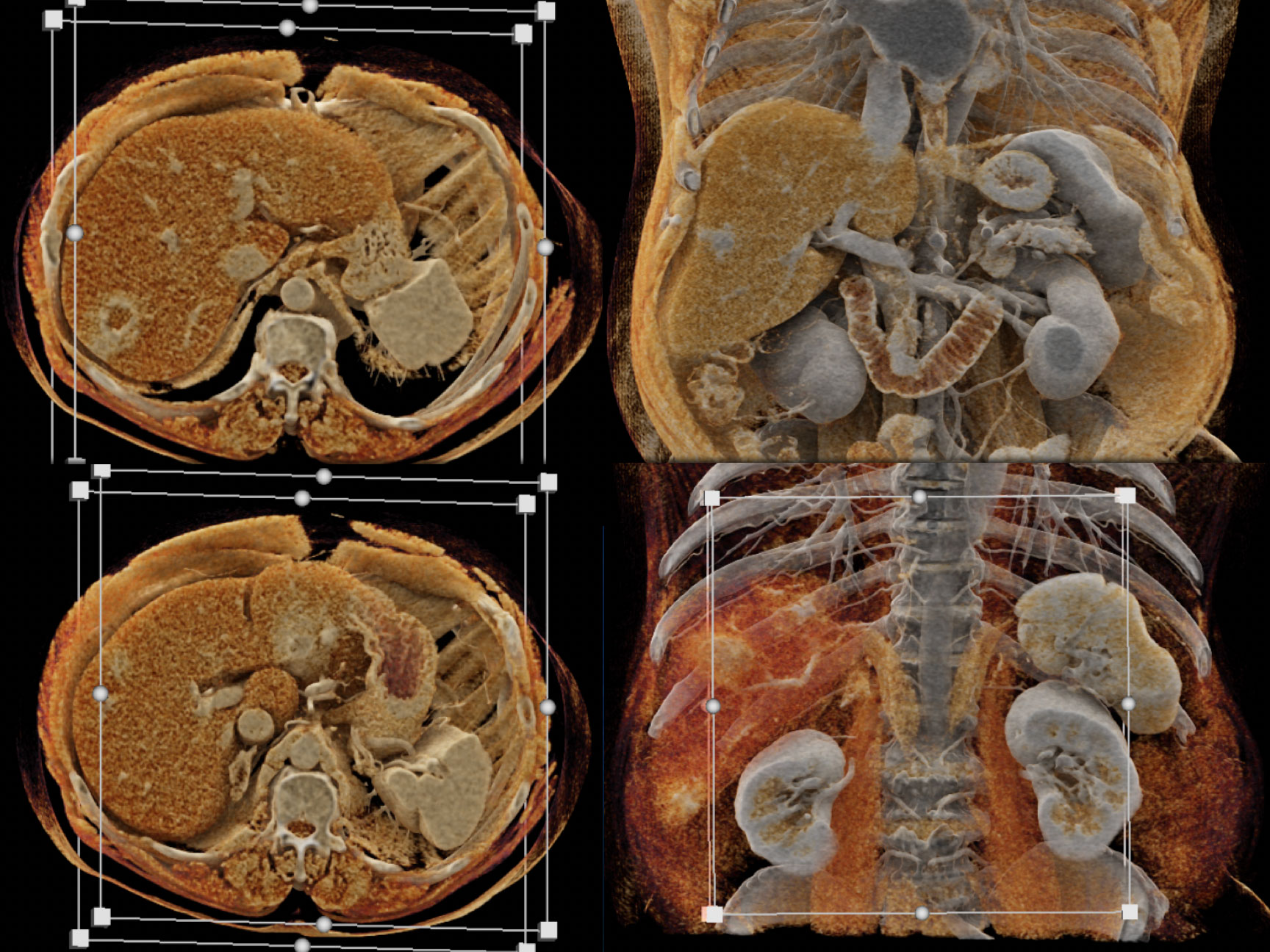 |
Neuroendocrine Tumor with liver metastases shown on both arterial and venous phase imaging. 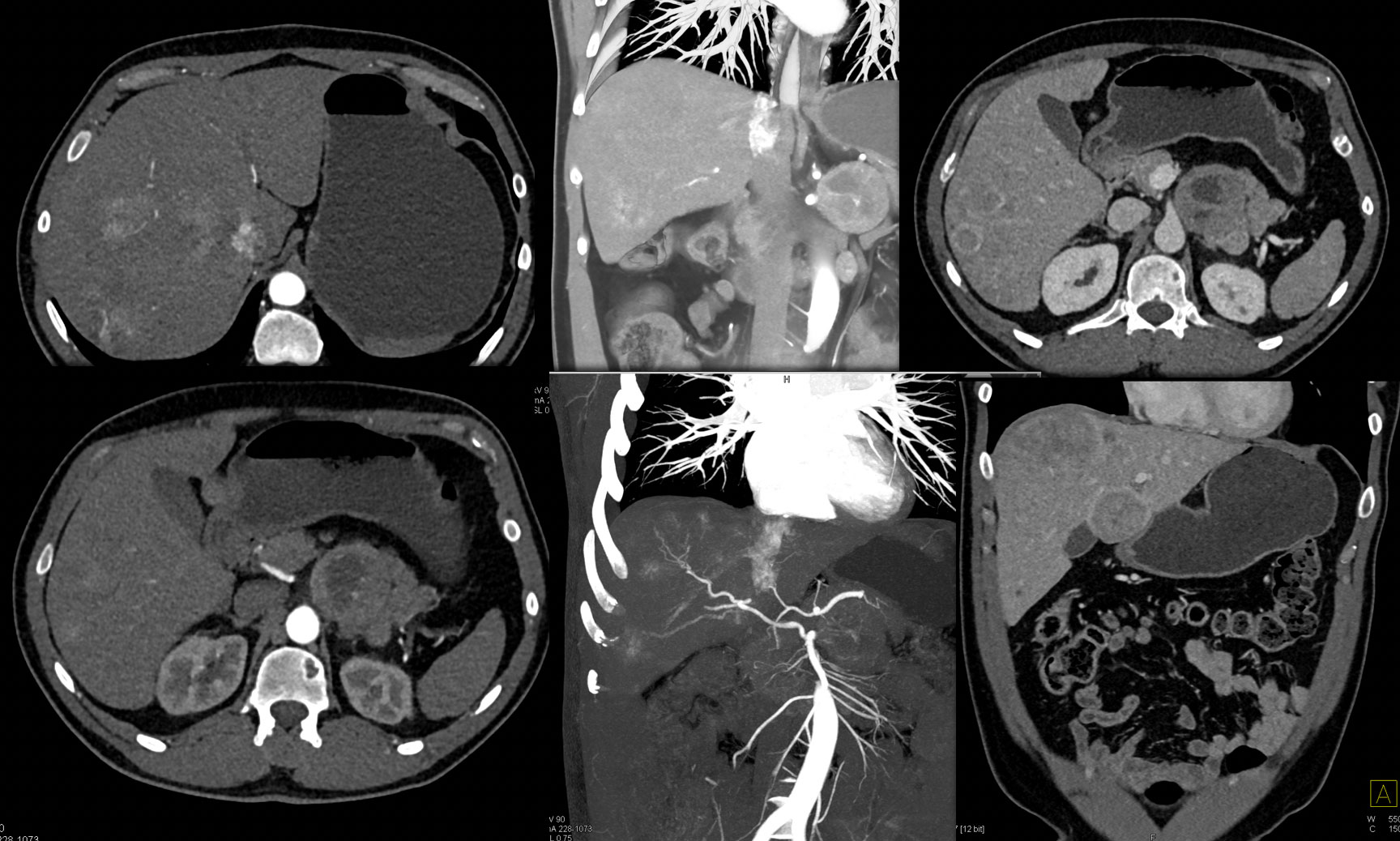 |
CR nicely defines the extent of liver metastases on a range of CR presets 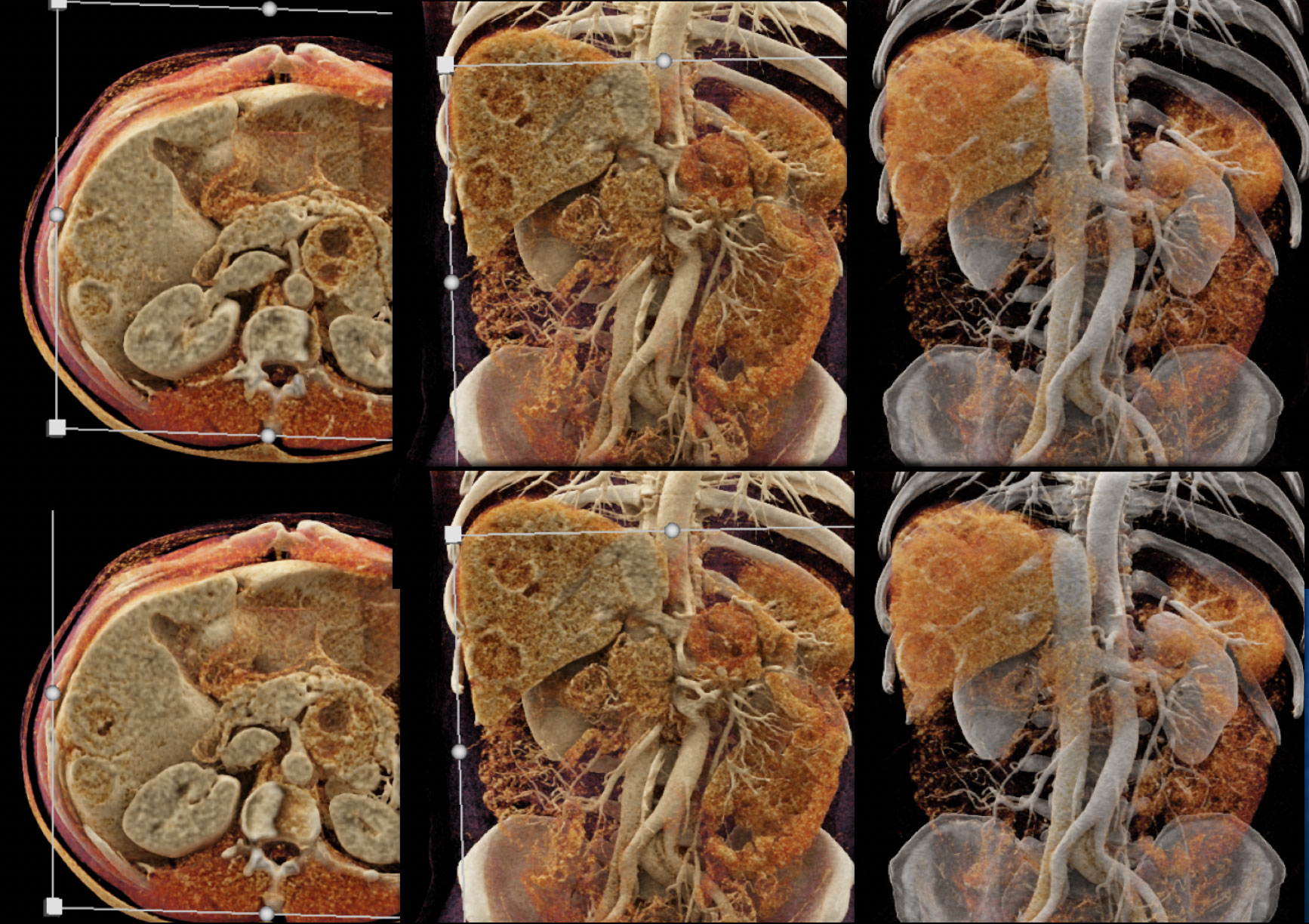 |
Pitfall: Adenosquammous Carcinoma of the Pancreas with Liver Abscess Post Op (Klebsiella and Enterococcus) simulating tumor recurrence. Perfusions changes well defined.  |
CR images nicely define the perfusion changes around the abscesses. 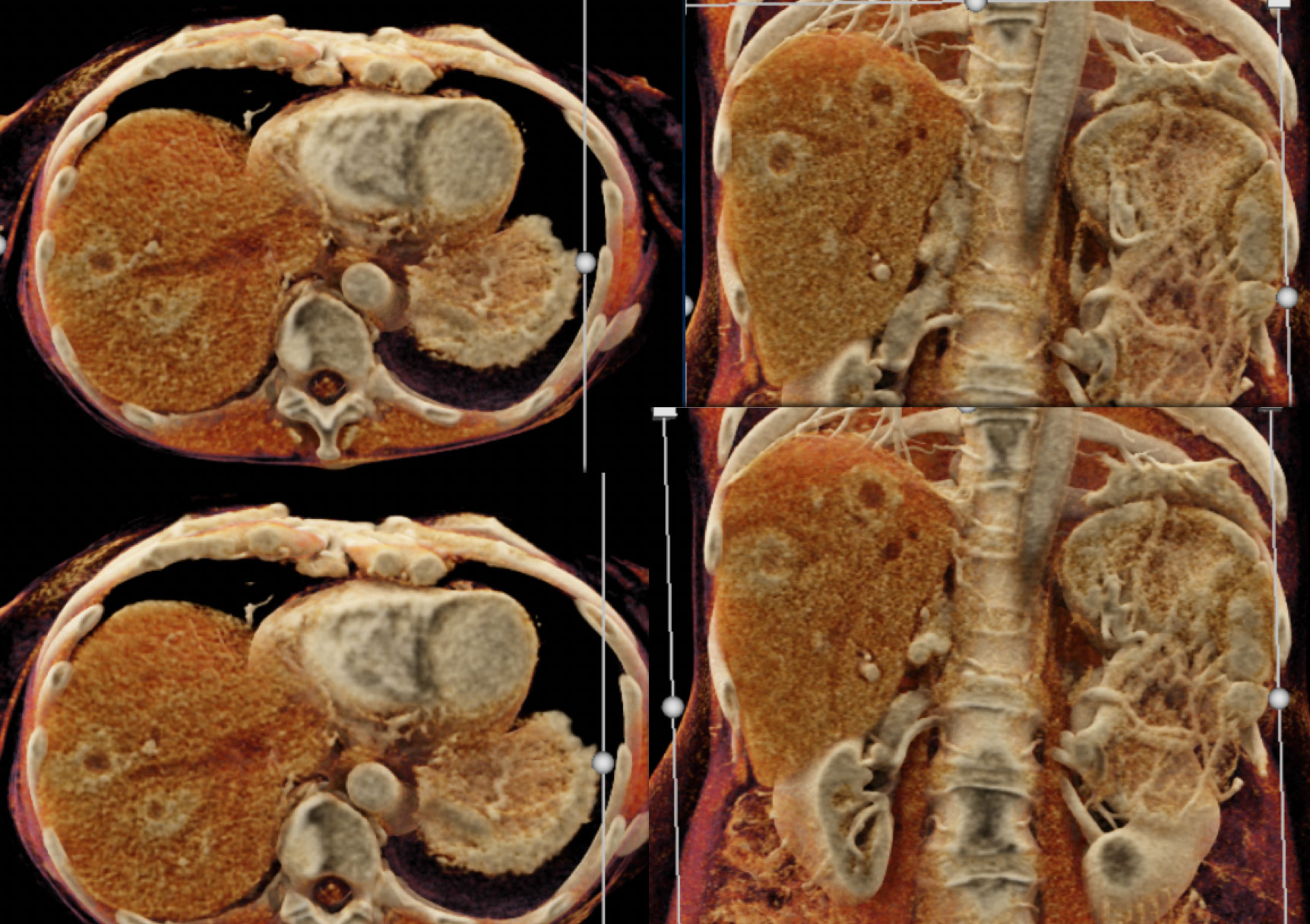 |
Conclusion and Next Steps The future of cinematic rendering for applications like liver tumor imaging include;
|
