MDCT of Duodenal Emergencies: Utility of 2D MPRs and 3D Rendering for Challenging But Critical DiagnosesMDCT of Duodenal Emergencies: Utility of 2D MPRs and 3D Rendering for Challenging But Critical Diagnoses Elliot K. Fishman, MD, FACR |
Duodenal Anatomy
|
Duodenal Anatomy 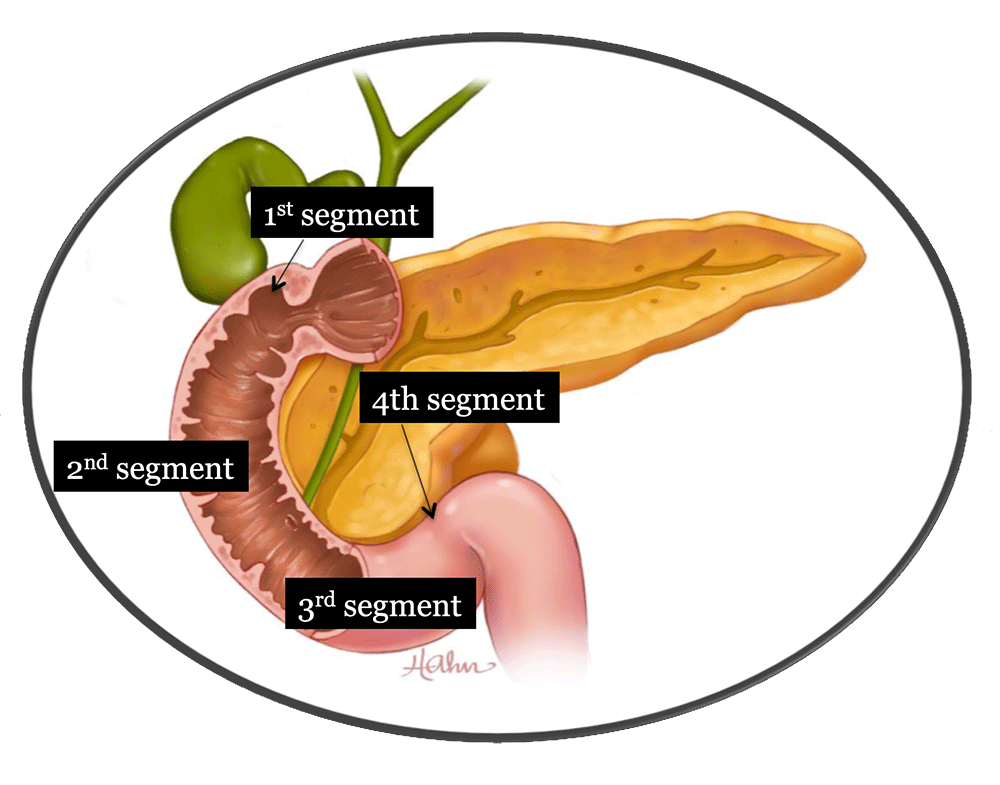 |
Severe Duodenitis 40 year old man admitted with epigastric and chest pain. Patient reported a history of alcohol abuse, H. pylori, NSAID use, and GERD. Coronal reconstructions help with distinguishing this from pancreatitis with resulting duodenitis. 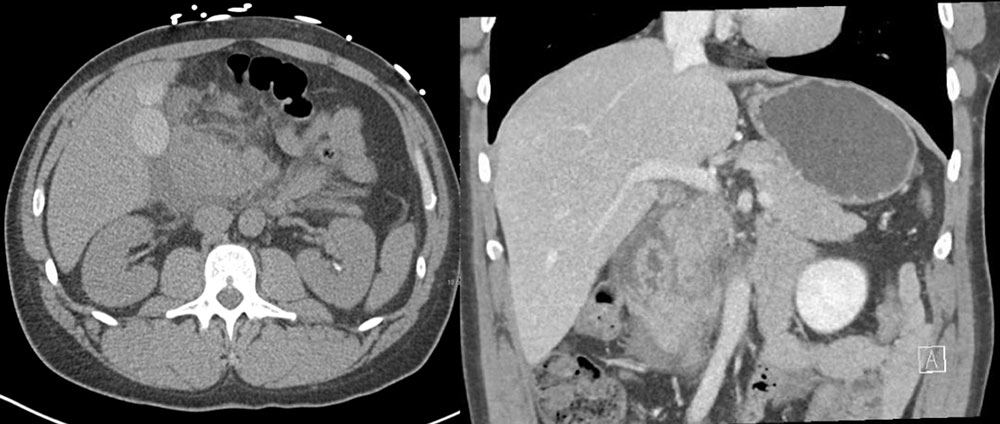 |
Duodenal Pneumatosis 24 year old woman with Rett Syndrome presenting with abdominal distention and lactic acidosis. Axial and sagittal CT show pneumatosis (arrow) of the duodenum. Surgery found marked adhesions without evidence of duodenal necrosis. 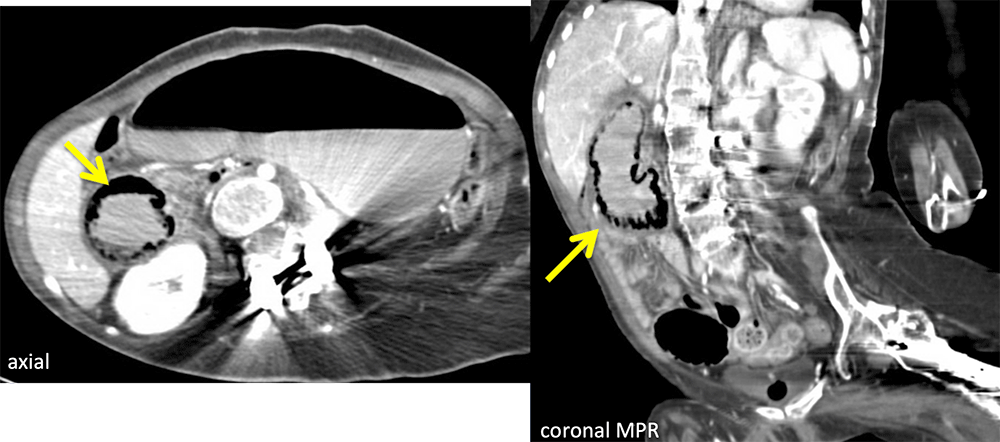 |
Perforated Duodenal Diverticulitis 62 year old woman presenting with sudden onset epigastric pain. CT shows obstructed duodenal diverticulum (D), with extensive mesenteric stranding (red arrows) and extraluminal gas (circle). 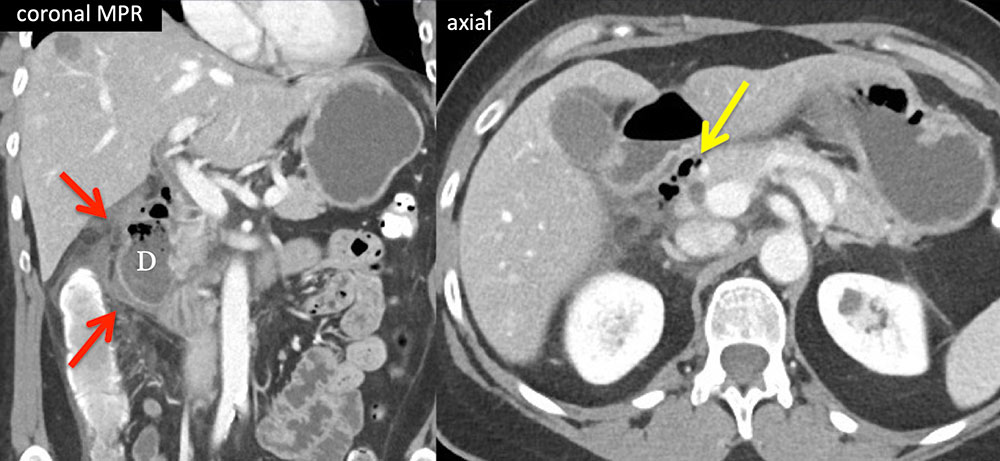 |
ERCP Duodenal Perforation 64 year old male with abdominal pain after ERCP. Axial CT shows extraluminal gas reflecting a duodenal perforation. This is the characteristic pattern of retroperitoneal and intraperitoneal free gas (arrows) seen in the setting of duodenal perforation. 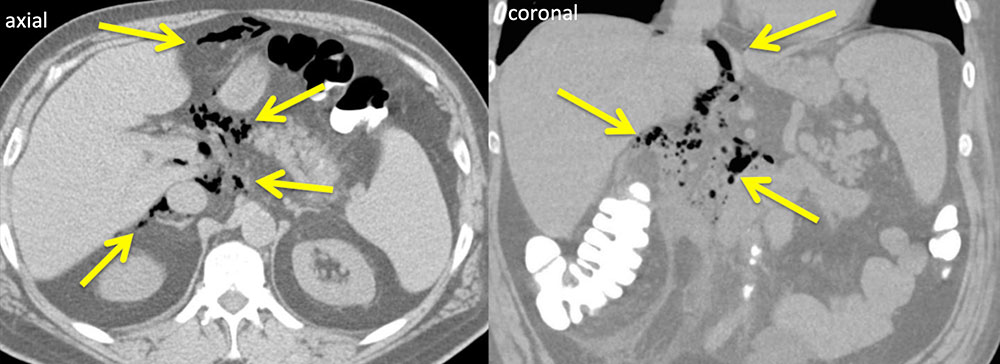 |
ERCP Duodenal Perforation 50 year old woman with significant post-procedure pain after EUS/ERCP. Axial and coronal CT with IV contrast shows a collection of extraluminal gas (arrows) adjacent to the 2nd and 3rd segments of the duodenum with a large amount of ascites tracking throughout the right side of the retroperitoneum. 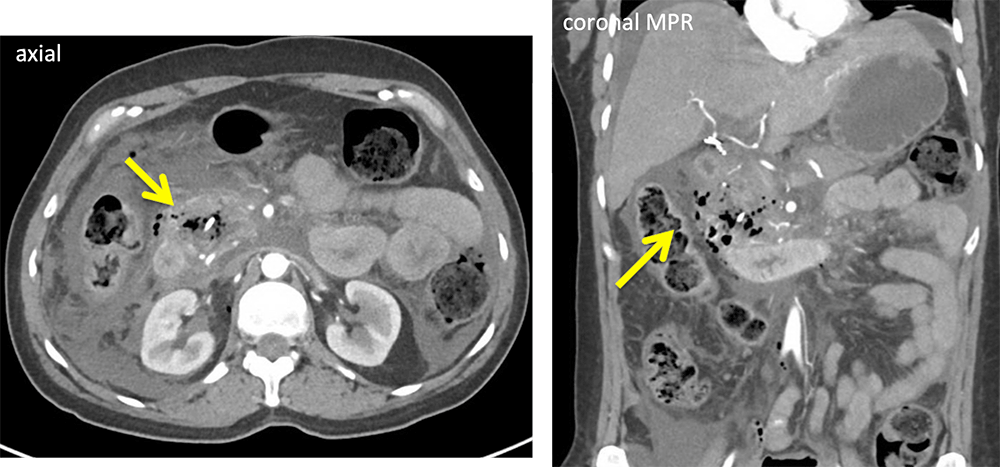 |
Perforated Ulcer 81 year old woman with contained perforation from duodenal ulcer. Axial IV contrast enhanced CT shows periduodenal stranding and small periduodenal collection (red arrow). Use of thin sections enables delineation of communication with duodenal lumen (yellow arrow). Emergency departments are commonly performing CT with water rather than positive oral contrast. Thin sections, MPRs and IV contrast facilitate visualization of gastrointestinal wall pathology. 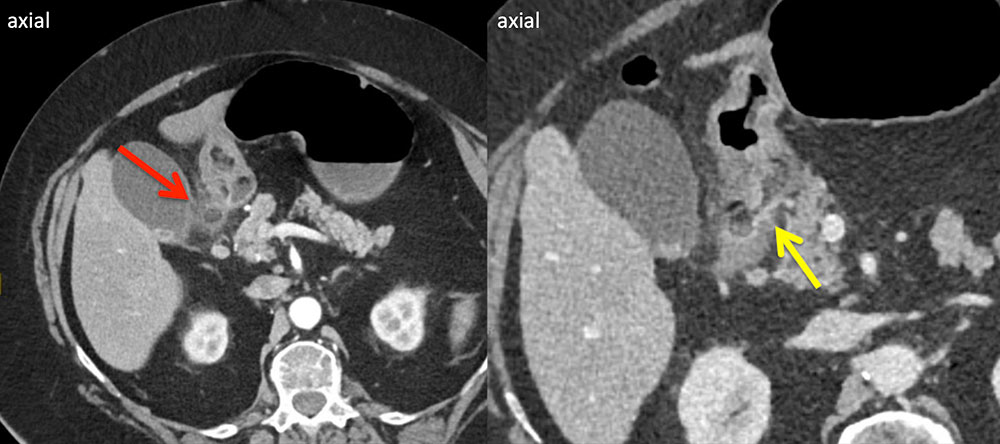 |
Acute Duodenal Perforation 81 year old woman with acute duodenal perforation. Oral and IV contrast enhanced CT shows free air, moderate ascites, disruption of the lateral wall of the duodenum (curved arrow) with a large perforation confirmed at surgery. 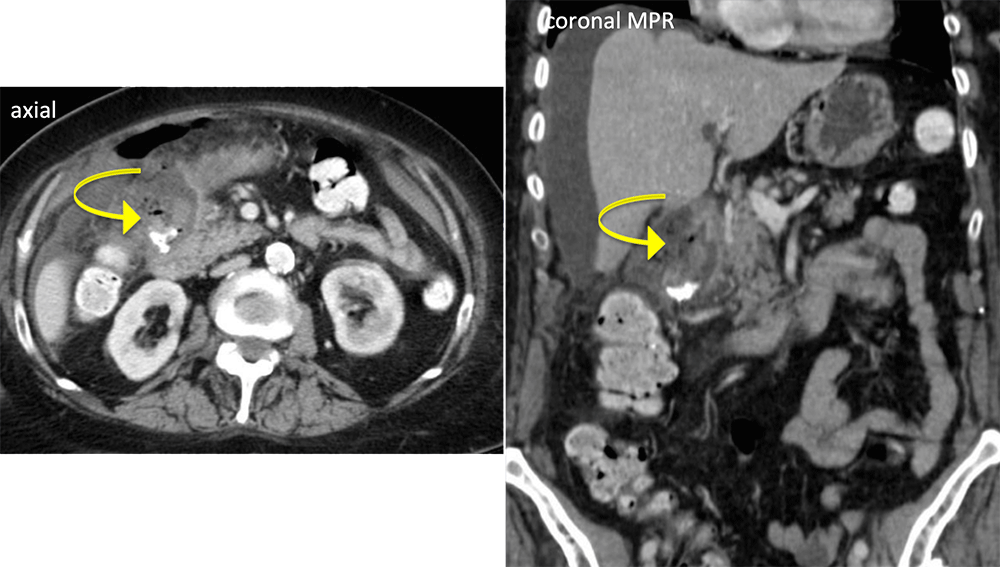 |
Duodenal Perforation 72 year old man presenting with sudden onset upper abdominal pain. Axial CT shows extraluminal oral contrast adjacent to the duodenum. Coronal MPR reconstruction shows the site of perforation along the lateral wall of the duodenum (red arrows) and extravasated PO contrast tracking into the right paracolic gutter (yellow arrows). 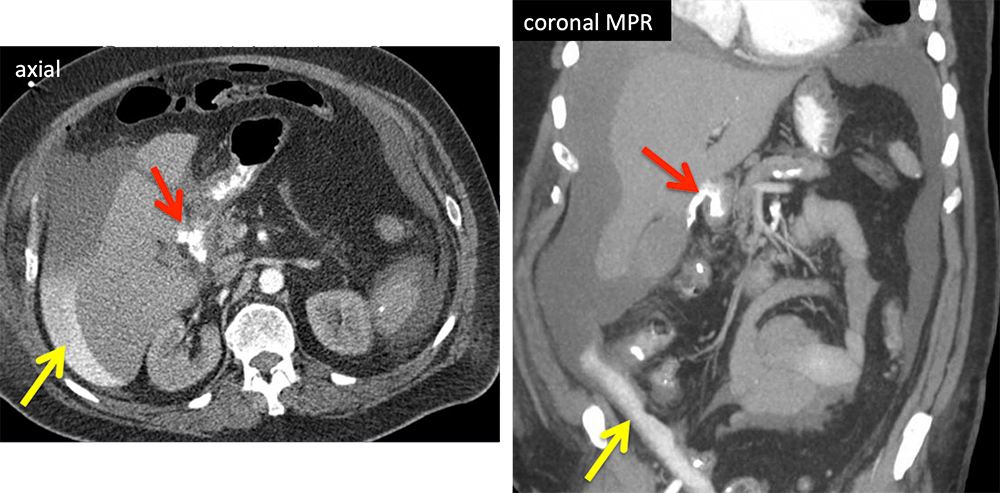 |
Duodenal Laceration 39 year old man presents with stab wound to the abdomen. Axial images shows duodenal mural hematoma (red arrow) and hemoperitoneum (H). Coronl reconstruction demonstrates stranding (red arrows), hemoperiteum (H) in the right paracolic gutter and a few foci of extraluminal air (yellow arrow). Laceration of the first portion of the duodenum found intraoperatively. 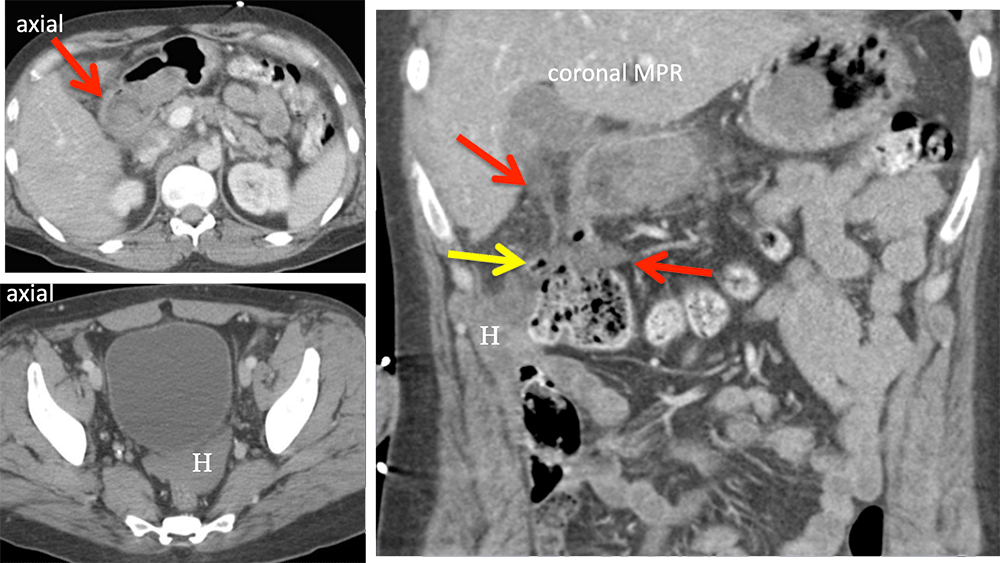 |
Duodenal Perforation by Fishbone Patient referred for pancreatic tumor. CECT shows thick walled multicystic mass between pancreas and duodenum (red arrows). Endoscopic US and aspiration disclosed infection (abscess). Small high density linear foreign body (yellow arrow) was a fishbone that perforated several weeks earlier (patient recounted episode of pain). 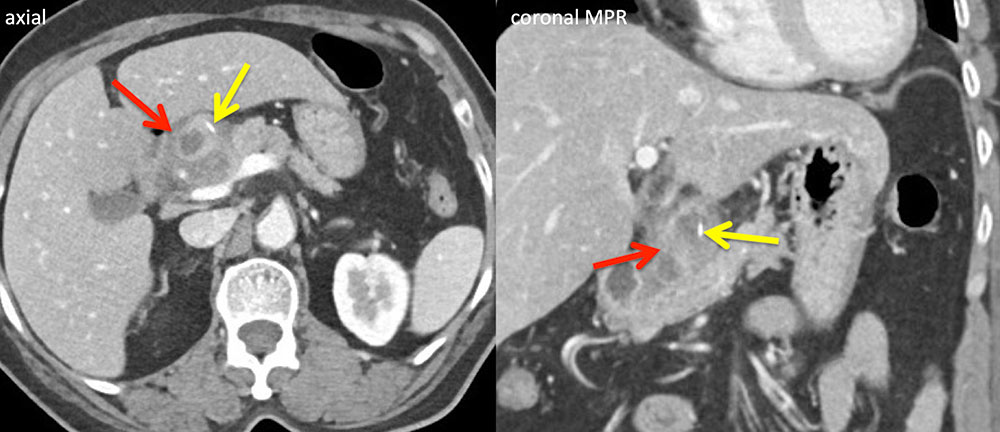 |
Duodenal Perforation by CBD Stent 22 year old woman with history of Crohn disease and primary sclerosing cholangitis. Patient developed acute abdominal pain, and coronal MPR and 3D VR show stent migrated through wall of duodenum with extraluminal gas (red arrows). 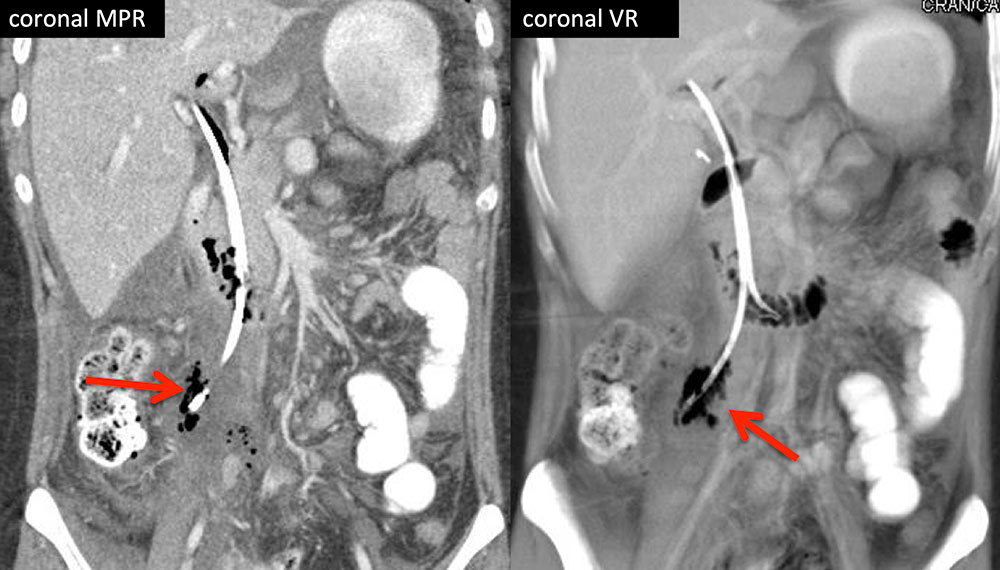 |
Duodenal Hemorrhage 69 year old woman with 3 days of melena following pancreaticoduodenectomy. Source of hemorrhage is a GDA pseudoaneurysm (arrows) bleeding into duodenum. The GDA stump is often the source of hemorrhage when post-Whipple patients develop GI bleeding, and this region should be carefully evaluated in axial and coronal planes. The absence of hemorrhage into the duodenal lumen does not diminish the critical nature of this finding. This patient was asymptomatic at time of scan, but nonetheless, was sent directly to the ED. She decompensated soon thereafter while being consented for interventional embolization due to acute rupture, but was successfully treated by IR coil embolization and discharged several days later. 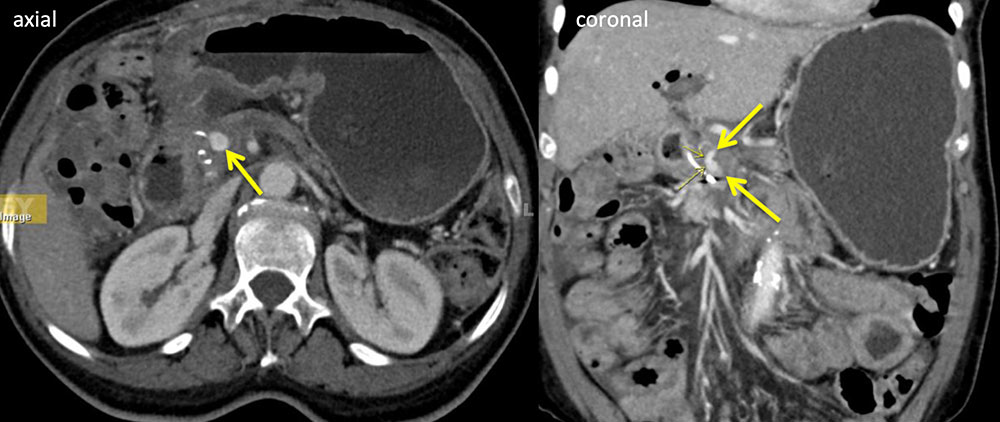 |
Active Hemorrhage into Duodenum 75 year old woman status post right hemicolectomy and partial duodenectomy who developed post-operative upper GI bleeding. CECT revealed active hemorrhage (arrows) into the D2 segment, increasing from arterial to venous phase, as well as an intraluminal hematoma (H). Patient was managed with GDA coil embolization. 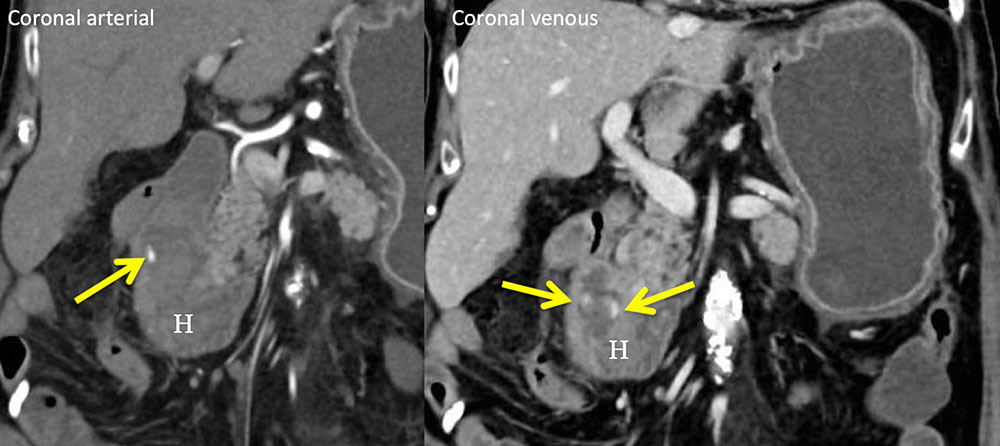 |
Duodenal Hematoma 25 year old man with acute abdominal pain while on anticoagulation. Noncontrast CT shows high density mass (H) in duodenal wall consistent with acute hematoma. 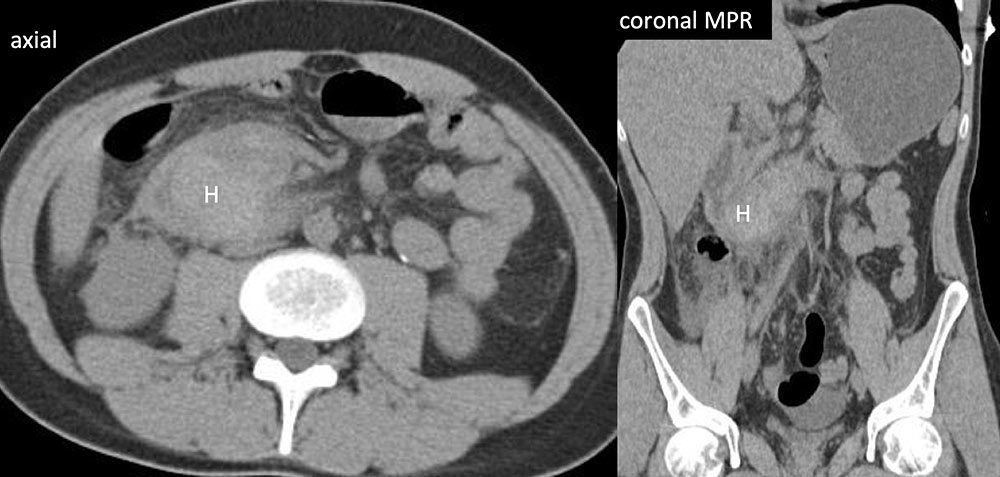 |
Duodenal Hematoma 62 year old woman with large duodenal hematom (arrows) on axial and coronal CT with IV and oral contrast. Relationship to duodenum (D) best depicted on coronal MPRs, essential to not mistake this important diagnosis for a pancreatic mass. 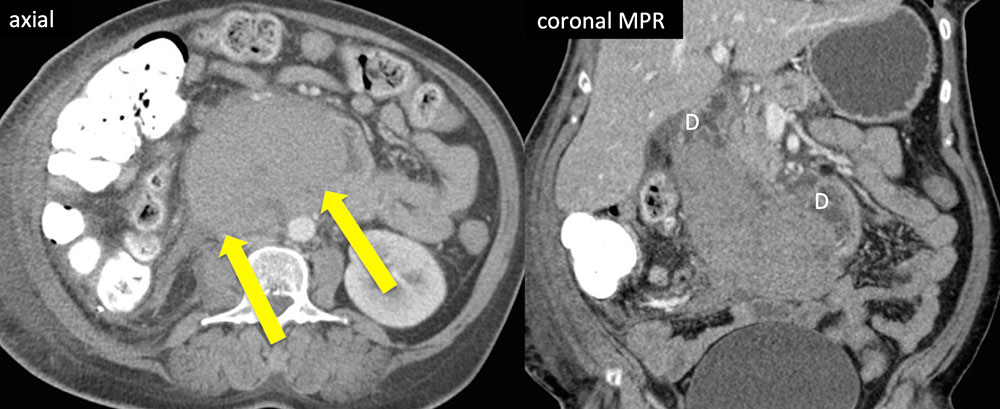 |
Aortoduodenal Fistula Rare complication of abdominal aortic aneurysm, which can occur before and after repair if EVAR is complicated by refractory endoleak. 87 year old female with CAD, AAA s/p endoluminal repair and revision who presented with progressive weakness. She was found to be severely anemic with baseline hemoglobin of 6 due to fistula between aneurysm sac and adjacent duodenum (arrow). Presence of gas in the aneurysm sac increases diagnostic confidence; however, this finding is not always identified desipte presence of a fistulous connection. 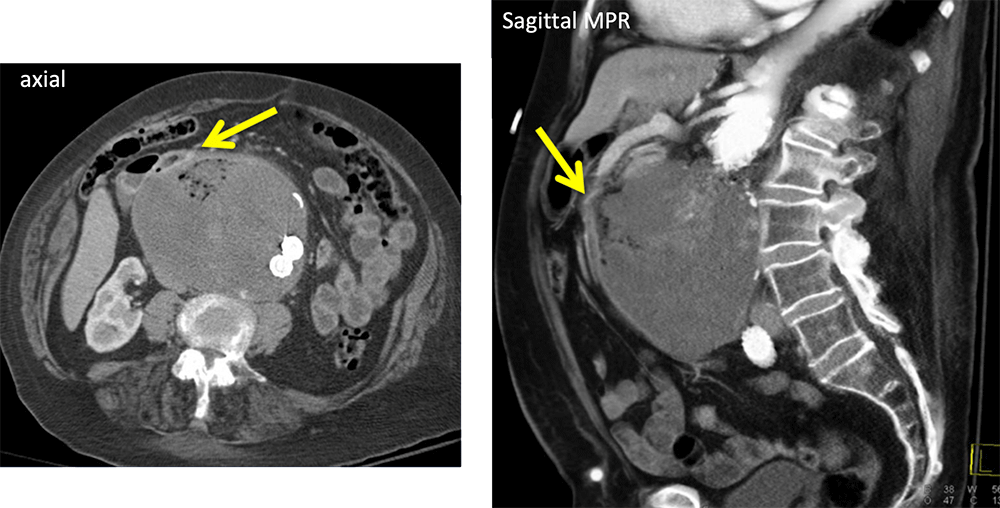 |
Pancreatic Adenocarcinoma 77 year old woman presenting with nausea and vomiting. CT revealed a mass in the body of the pancreas with extension to the stomach and duodenum (D). Note the upstream dilatation of the duodenum and stomach. 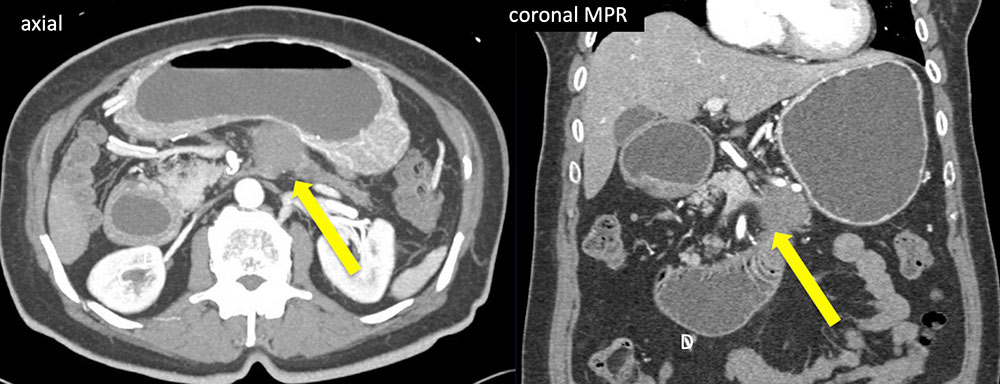 |
Duodenal Adenocarcinoma 77 year old man with fatigue and nausea found to have obstructing duodenal adenocarcinoma (arrow). Note the upstream dilation of the more proximal duodenum (D) and stomach (S). 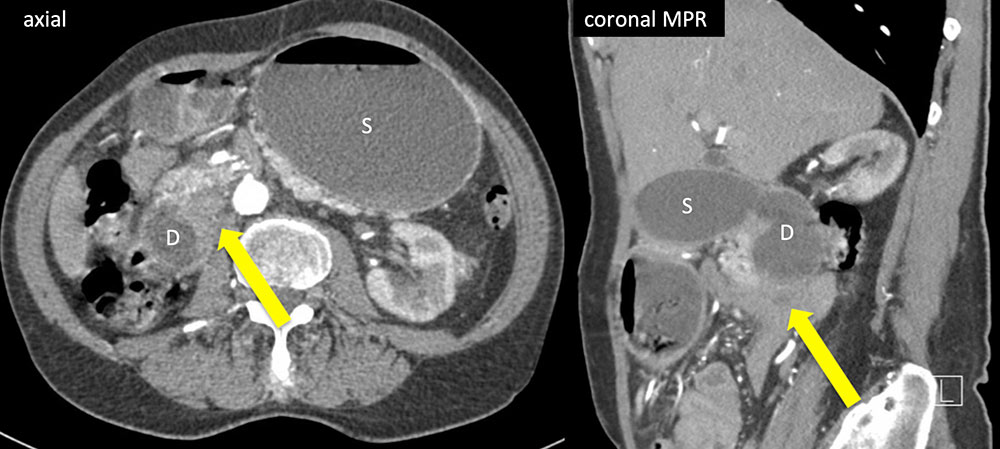 |
References
|
References
|
