CT of Uncomplicated and Complicated Gastric Volvulus: Unraveling the Imaging Findings with Volumetric Dataset InterpretationsCT of Uncomplicated and Complicated Gastric Volvulus: Unraveling the Imaging Findings with Volumetric Dataset Interpretations |
Gastric Volvulus
|
Gastric Volvulus
|
Organoaxial Volvulus
 |
Mesenteroaxial Volvulus
 |
Acute Gastric Volvulus
|
Complications of Acute Volvulus
|
Imaging of Gastric Volvulus
|
MDCT of Complicated Volvulus
|
MDCT of Complicated Volvulus
|
MDCT of Complicated Volvulus
|
MDCT of Complicated Volvulus
|
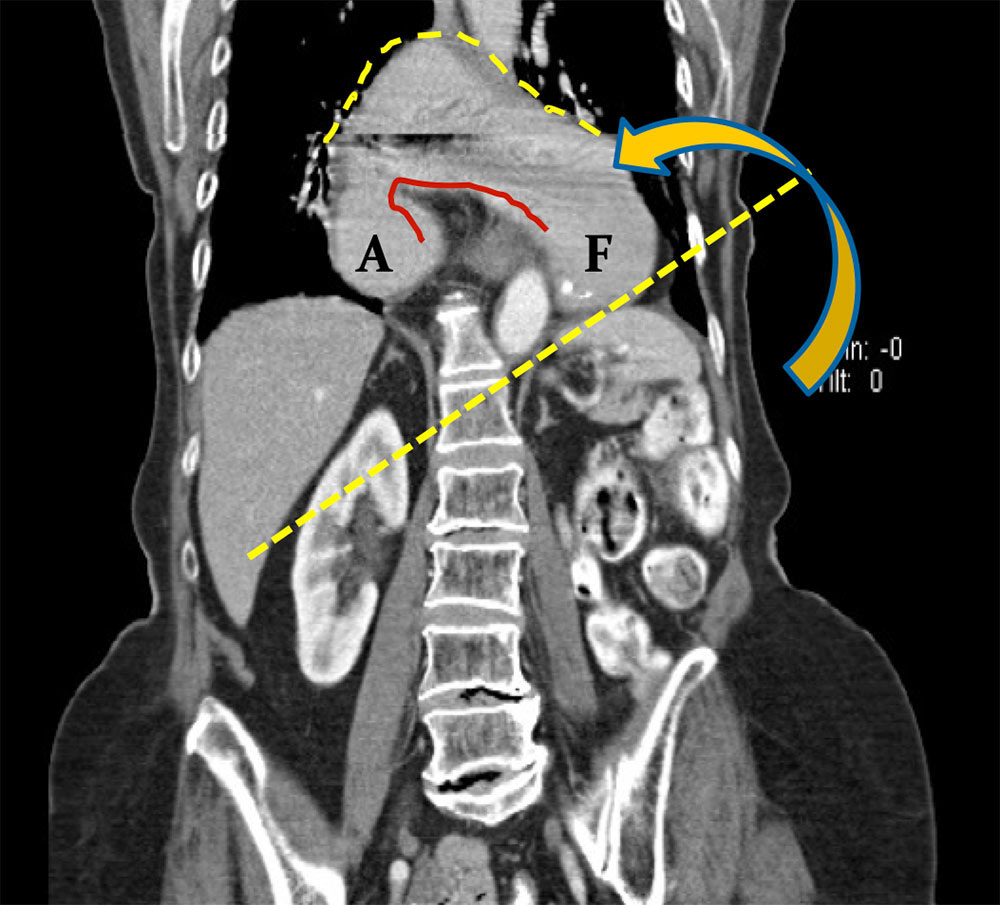
Case 1. Organoaxial Coronal MPR from IV contrast enhanced MDCT shows uncomplicated organoaxial gastric volvulus, secondary to a complete hiatal hernia. A= antrum F= fundus 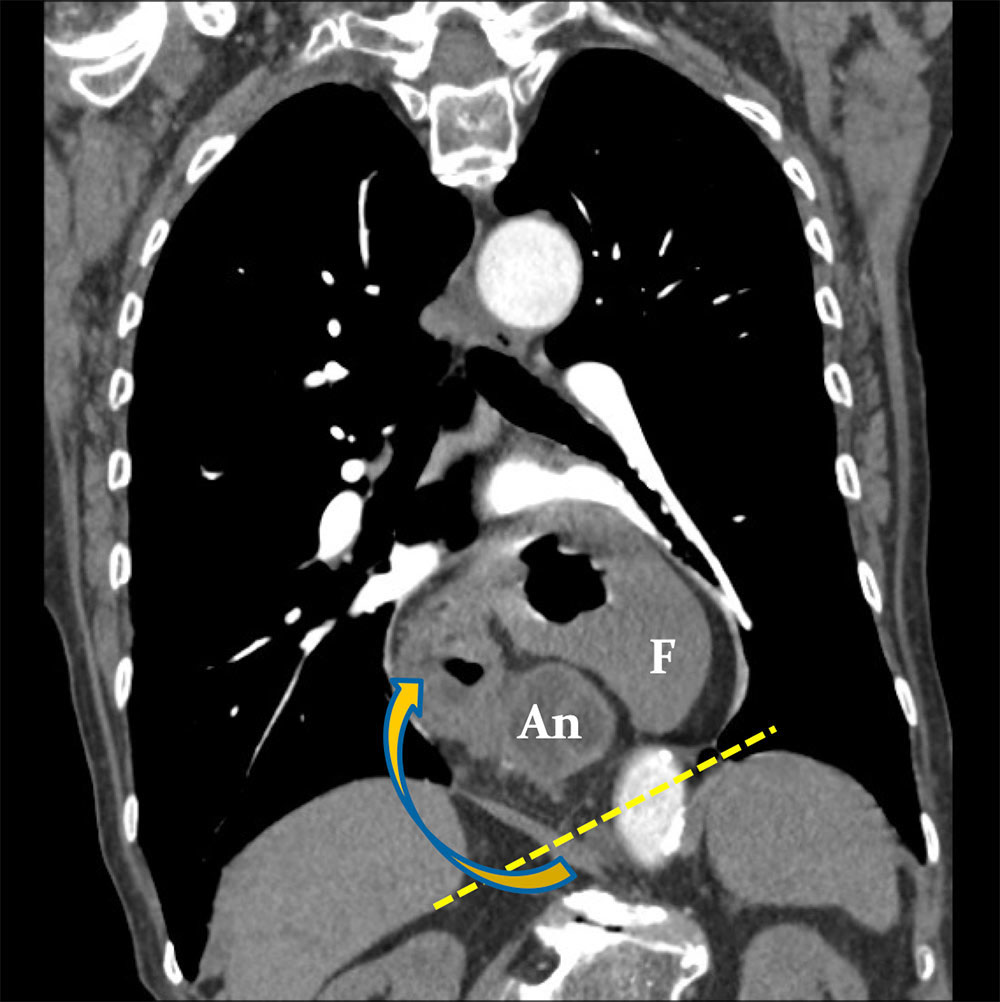 |
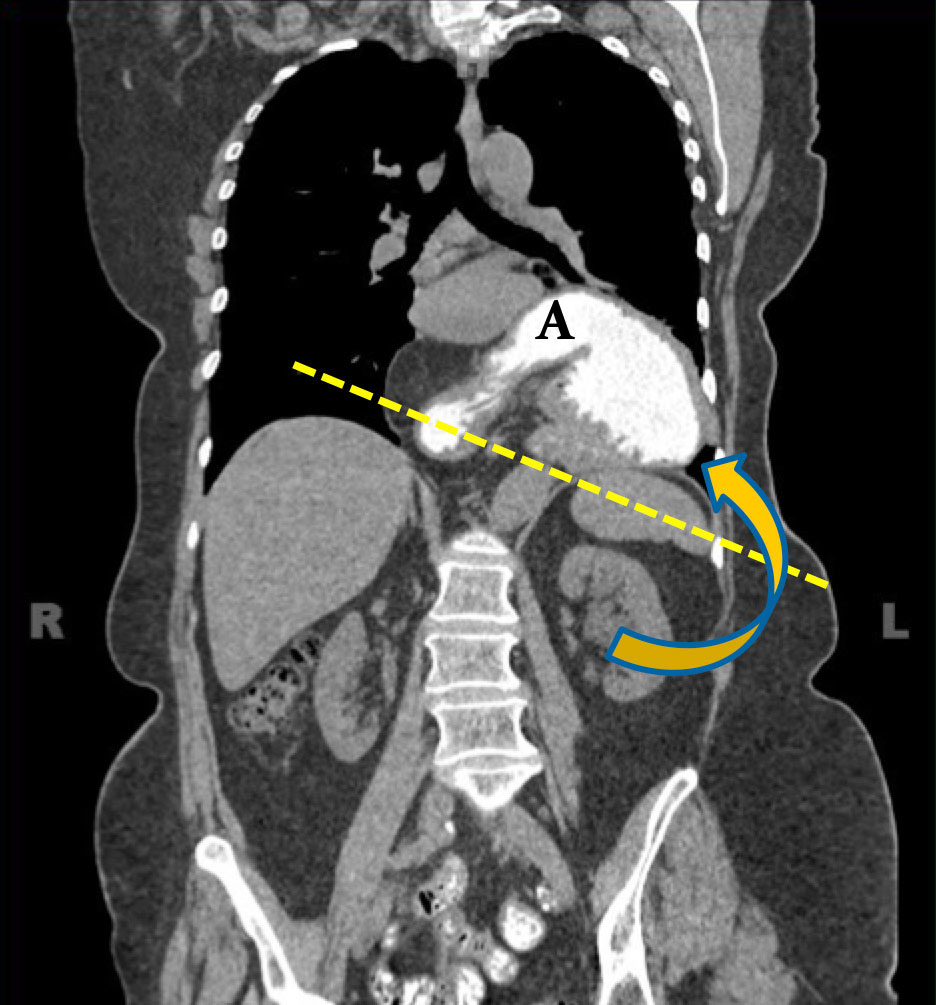
Case 2. Mesenteroaxial Coronal MPR from IV contrast enhanced MDCT shows uncomplicated chronic mesenteroaxial gastric volvulus, secondary to large diaphragmatic hernia. An= antrum F= fundus 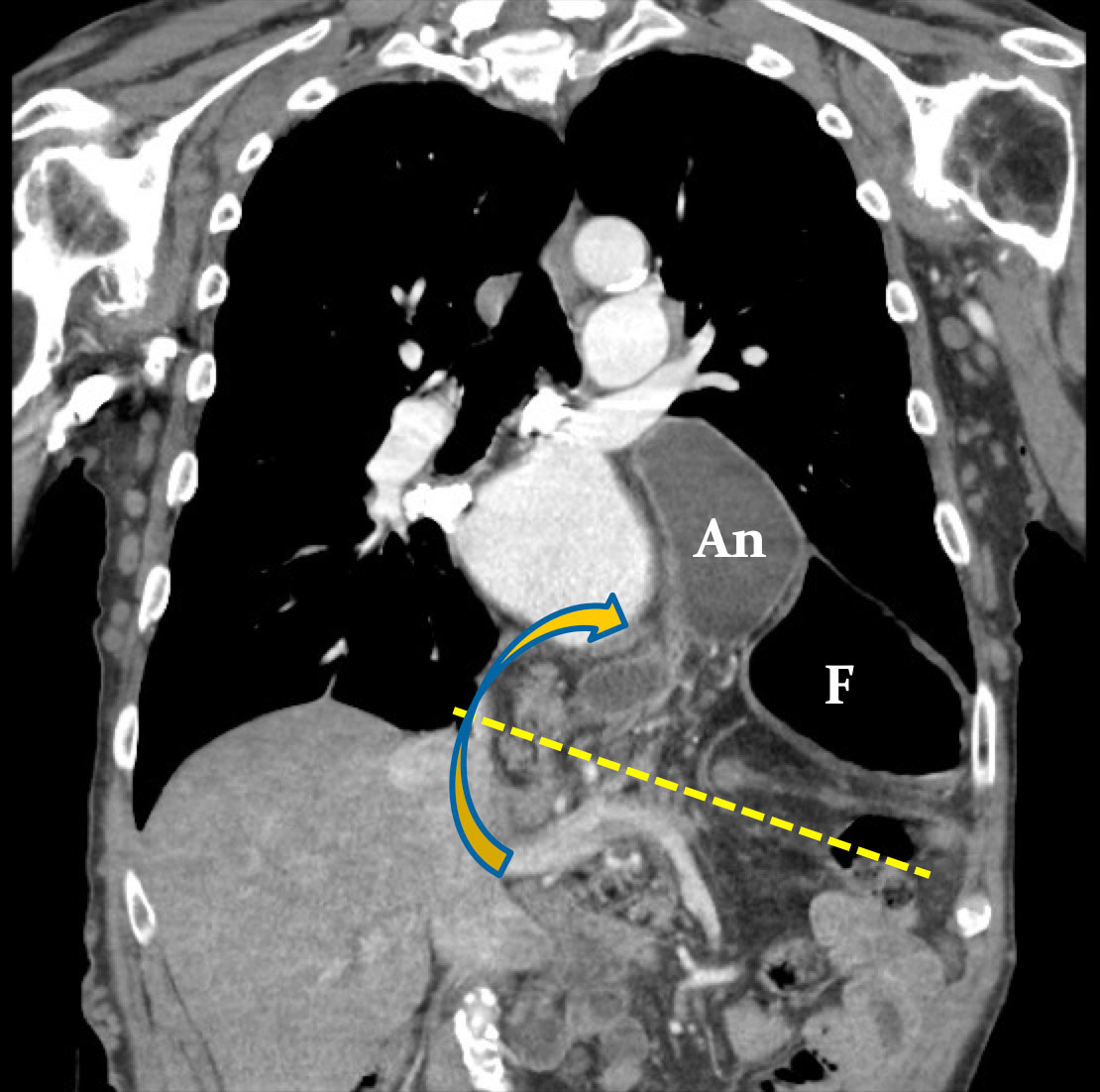 |
Case 3. Organoaxial Coronal MPR from noncontrast MDCT shows uncomplicated organoaxial gastric volvulus, secondary to a large hiatal hernia. 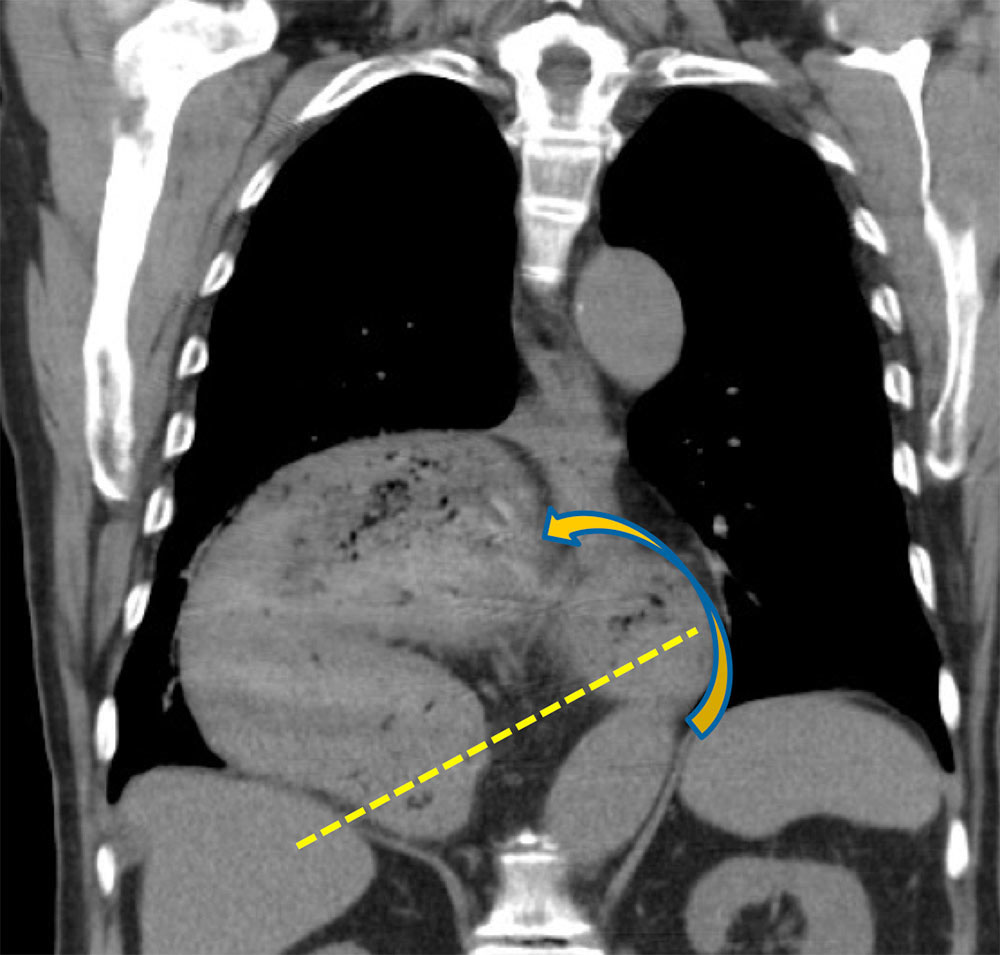 |
Case 4. Mesenteroaxial Coronal MPR from IV contrast enhanced MDCT (A) of chronic uncomplicated mesenteroaxial gastric volvulus, secondary to large diaphragmatic hernia. (B) Subsequent Upper GI examination. 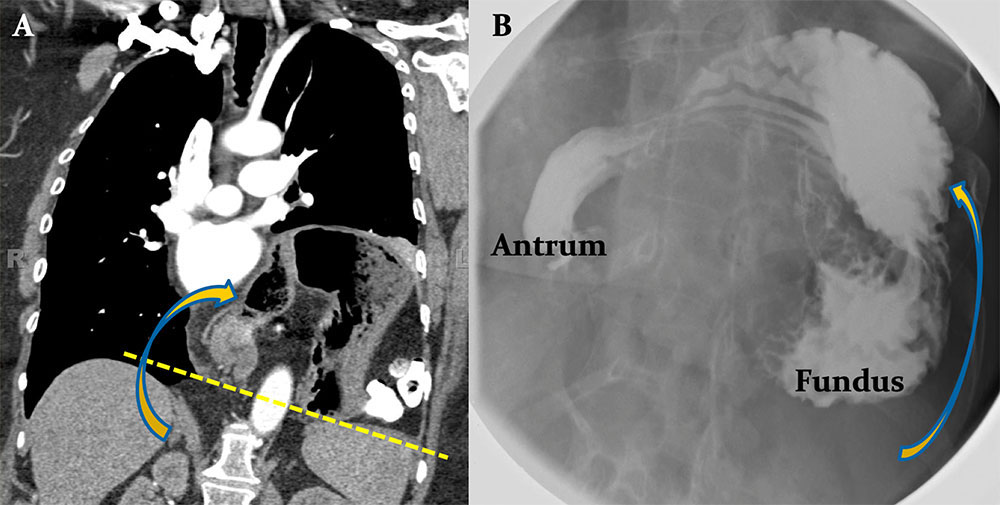 |
Case 5. Organoaxial Coronal MPR (A) and axial image (B) from oral and IV contrast enhanced MDCT shows uncomplicated organoaxial gastric volvulus, secondary to a large hiatal hernia. 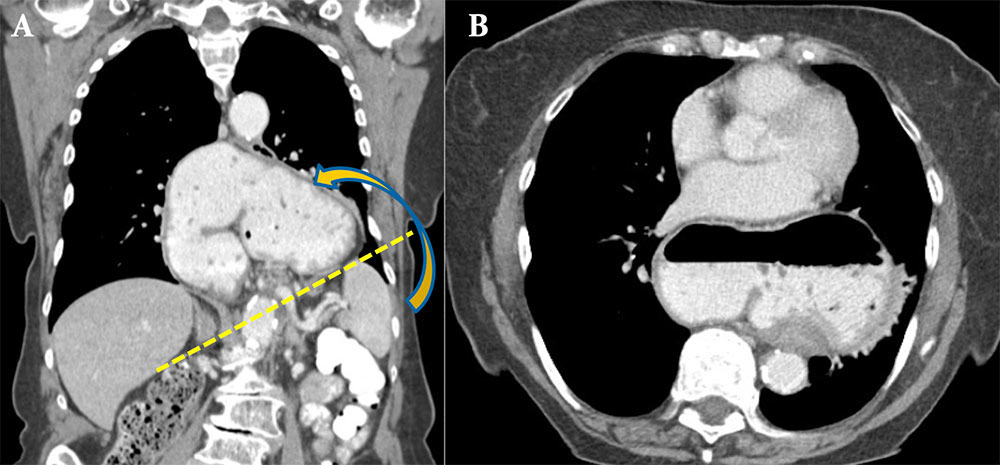 |
Case 6. Mesenteroaxial Coronal (A) and sagittal (B) MPRs from oral contrast enhanced MDCT show uncomplicated mesenteroaxial gastric volvulus, secondary to large diaphragmatic hernia. Notice the antrum (An) lying above the fundus (F). 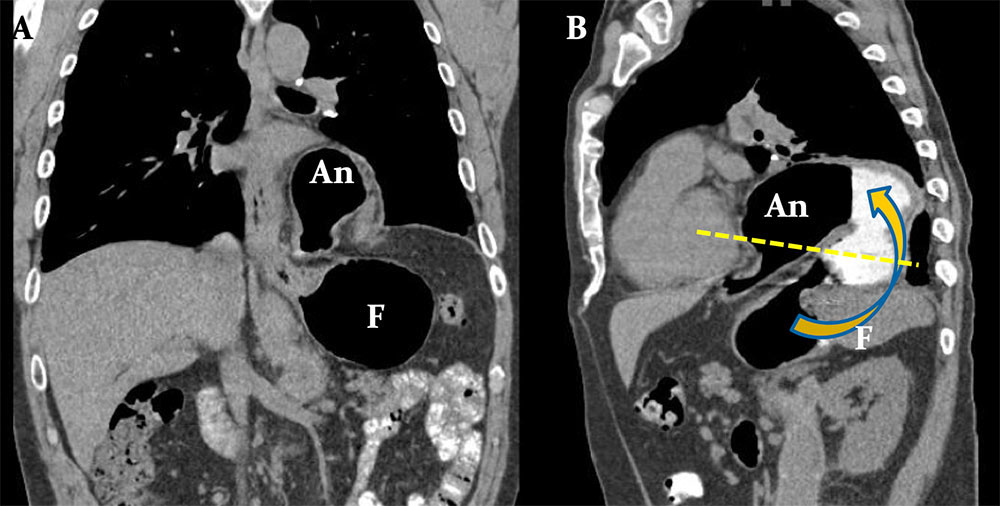 |
Case 7. Chronic Mixed Type Volvulus Coronal (A) and sagittal (B) MPRs from oral contrast enhanced Chronic gastric volvulus of the mixed / combined type. Sagittal (A) and coronal (B) MPRs from IV contrast enhanced MDCT show complex twisting and turning of the stomach, but not along any particular axis. The cause is secondary to eventration and elevation of the posterior diaphragm. 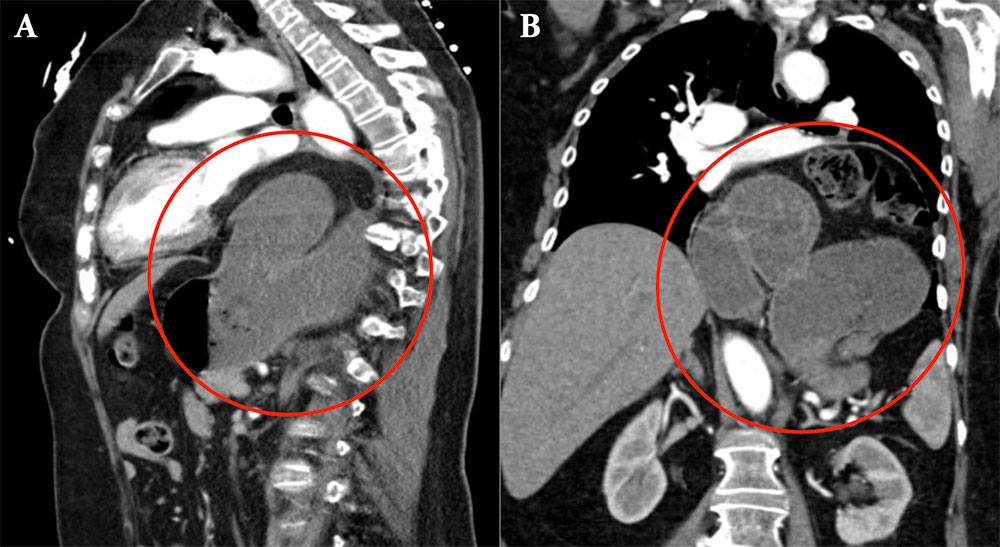 |
Case 8. Mixed Type Volvulus Axial image (A) and coronal MPR (B) from IV and oral contrast enhanced MDCT demonstrate complex turning of the stomach (circle), but not along any particular axis, compatible with a mixed type volvulus. 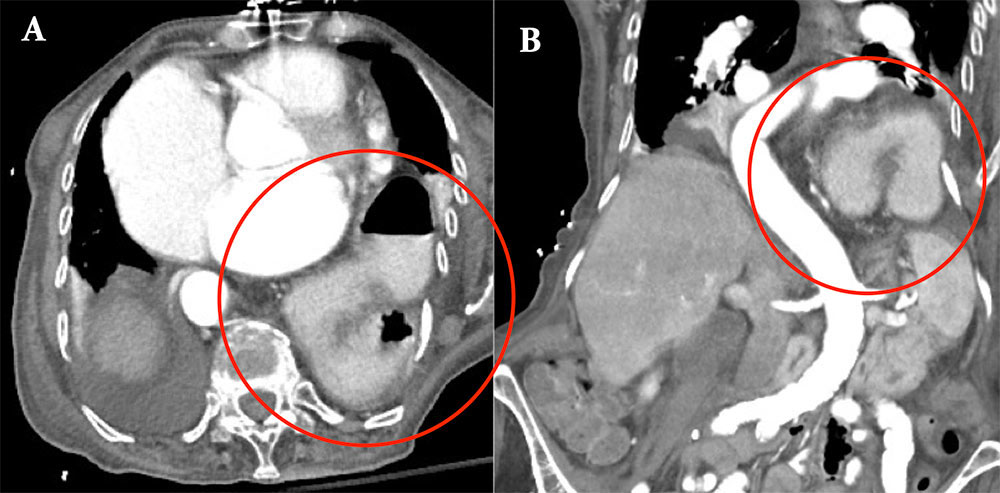 |
Case 9. Mixed Type Volvulus Axial image (A) and sagittal MPR (B) from IV contrast enhanced MDCT in a patient with recurrent mild abdominal symptoms demonstrate an uncomplicated mixed type volvulus (circle). 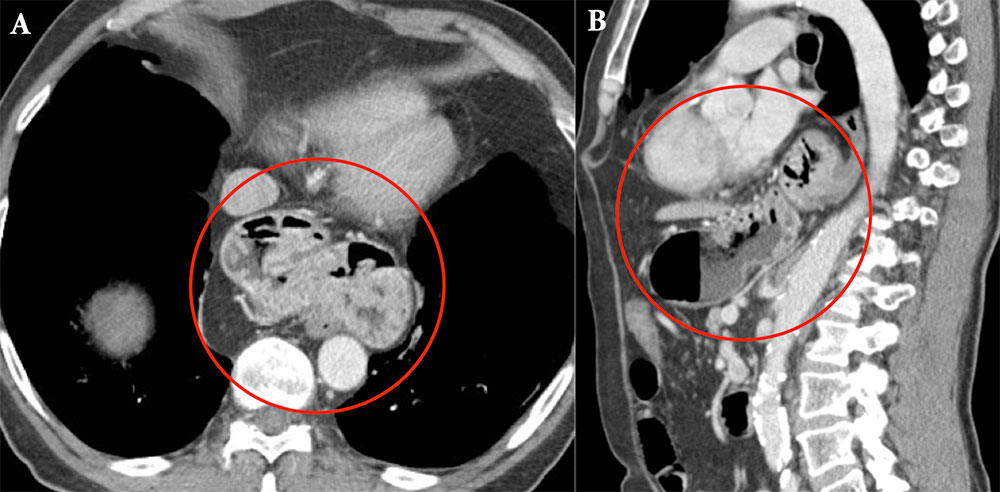 |
Case 10. Mixed Type Volvulus Coronal 3D volume rendering (A), coronal MPR (B) and axial image (C) from IV contrast enhanced MDCT demonstrate complex twisting of the stomach, but not along any particular axis, compatible with a mixed type volvulus. 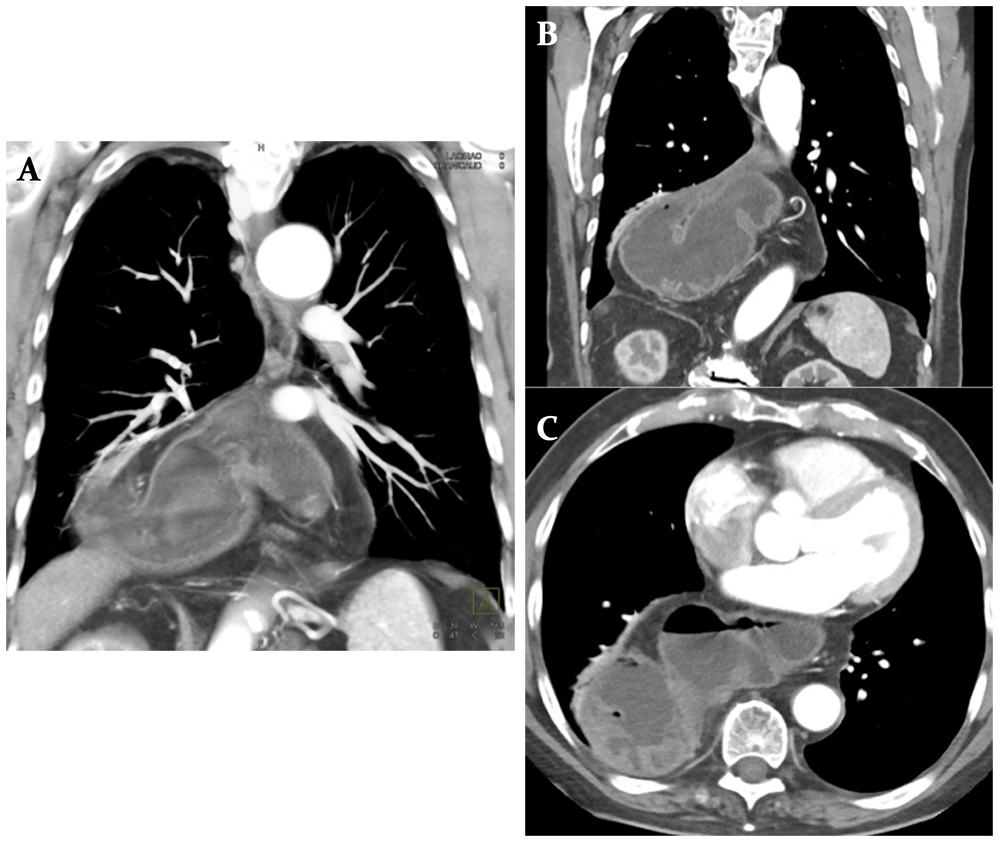 |
Case 11. Volvulus with Obstruction Coronal MPR (A) and axial image (B) from oral and IV contrast enhanced MDCT show organoaxial volvulus with outlet obstruction at the antropyloric region, narrowed by the distended body (arrow). Note the gastric distention with ingested material and air fluid level (*). No additional findings to suggest ischemia. 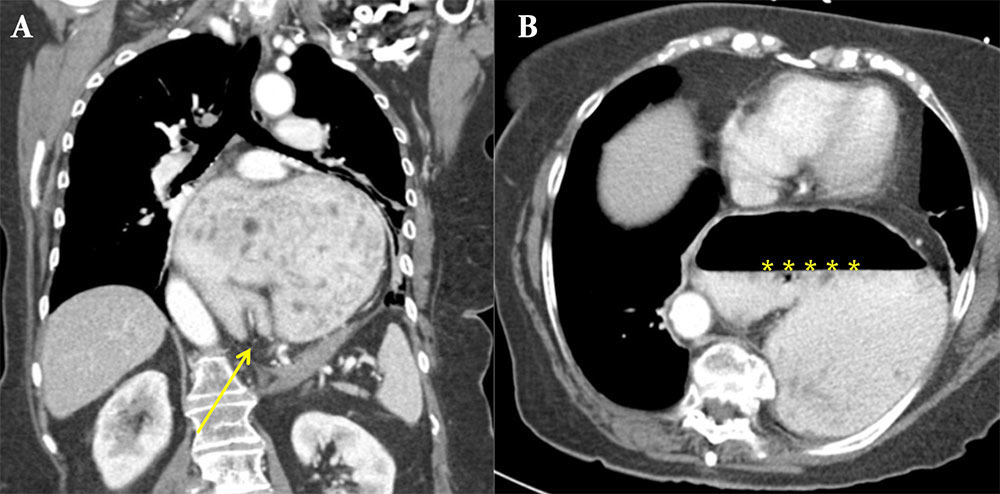 |
Case 12. Volvulus with Obstruction Coronal MPR (A), axial image (B) and coronal 3D volume rendering (C) from IV contrast enhanced MDCT show a large hiatal hernia with gastric volvulus and high grade outlet obstruction at the level of the antropyloric region (arrows). Again seen is gastric distention with air fluid level (*). 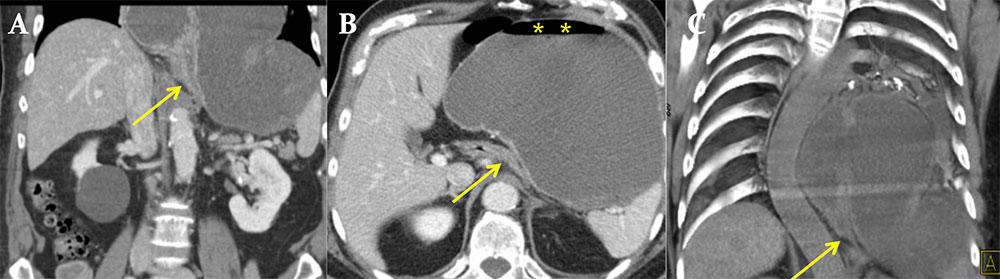 |
Case 13. Volvulus with Obstruction Coronal MPR from IV contrast enhanced MD CT baseline study (A) in a patient with chronic organoaxial gastric volvulus. Chest radiograph (B), axial oral and IV contrast enhanced MDCT (C,D) when patient developed acute outlet obstruction at the antropyloric region traversing through the esophageal hiatus (arrow). Gastric distention with air fluid level (*). An = antrum, F = fundus. 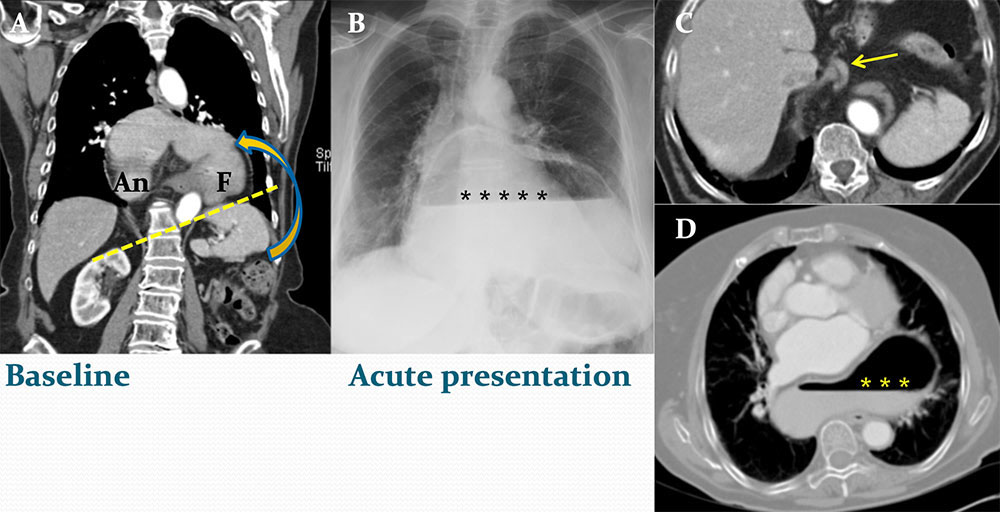 |
Case 14. Volvulus with Ascites Coronal MPR (A) and axial image (B) from IV contrast enhanced MDCT show organoaxial gastric volvulus with small amount perigastric ascites (arrows). There is no obstruction nor gastric wall thickening. Adjacent fluid as an isolated secondary finding is non specific; nonetheless, it is noteworthy and important to inform clinicians to correlate with symptoms, as intermittent strangulation is possible. 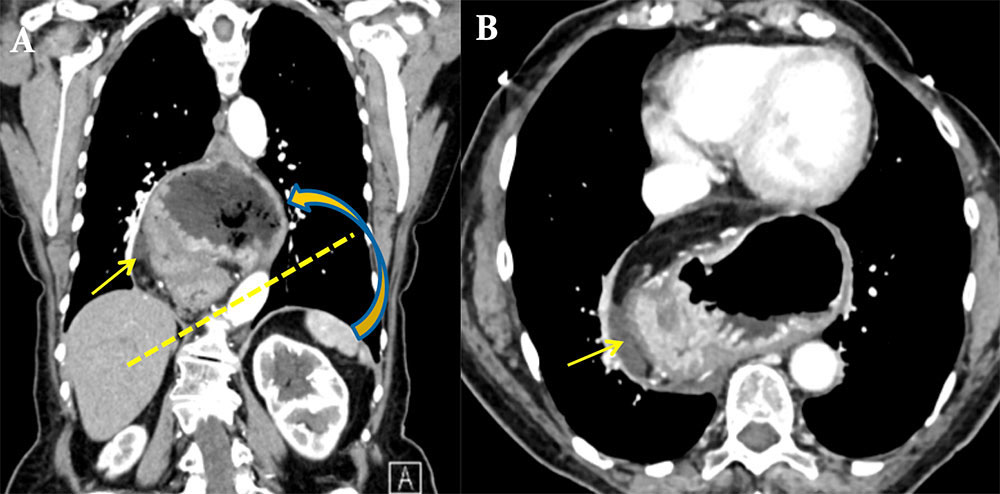 |
Case 15. Volvulus with Obstruction and Strangulation Baseline coronal MPR (A) from oral and IV contrast enhanced MDCT demonstrates large hiatal hernia with chronic volvulus (circle). Patient presented at follow up with acute abdominal pain. Axial image (B) and coronal MPR (C) from oral and IV contrast enhanced CT demonstrates luminal distention and gastric wall thickening (arrows), an indicator of strangulation in the setting of obstruction. 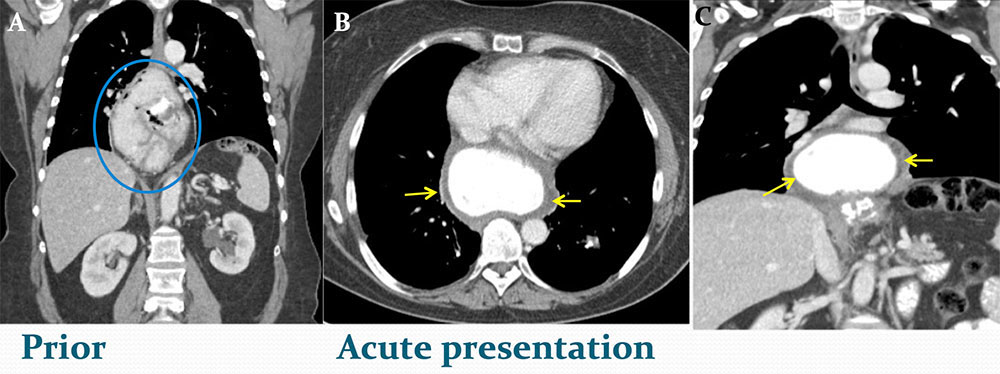 |
Case 16: Volvulus with Gastric Ischemia Axial image (A) and coronal MPR (B) from oral contrast enhanced MDCT show organoaxial volvulus with outlet obstruction and signs of ischemia, as evidenced by bowel walk thickening (solid arrow) and perigastric fluid (dashed arrow). No gastric emphysema. 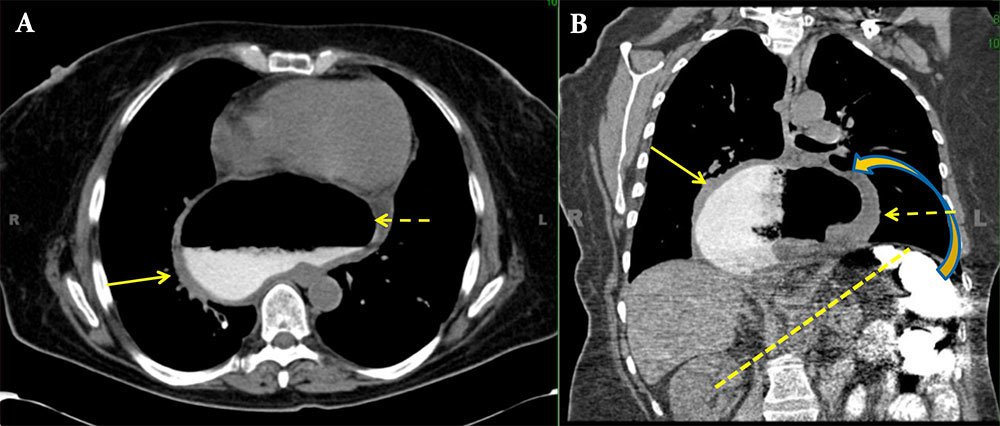 |
Treatment
|
Summary
|
References
|
