Pericardial Disease: A Resident Primer
Pericardial Disease: A Resident Primer Linda C. Chu The Russell H. Morgan Department of Radiology and Radiological Science, Johns Hopkins University, Baltimore MD |
Overview
|
Introduction
|
Pericardial Anatomy
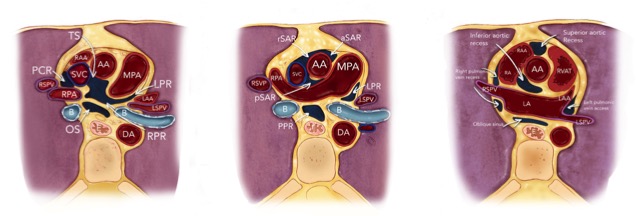
Broderick LS et al. RadioGraphics 2005;25(2):441-53. |
|
 Abbreviations: AA ascending aorta; aSAR anterior superior aortic recess; B bronchi; E esophagus; LA left atrium; LAA left atrial appendage; LPR left pulmonic recess; LSPV left superior pulmonary vein; MPA main pulmonary artery; OS oblique sinus; PCR postcaval recess; PPR posterior pericardial recess; pSAR posterior superior aortic recess; RA, right atrium; RAA right atrium appendage; RPA right pulmonary artery; RPR right pulmonic recess; RPVR right pulmonic vein recess; rSAR right superior aortic recess; RSPV right superior pulmonary vein; RVOT right ventricular outflow tract; SAR superior aortic recess; SVC superior vena cava Abbreviations: AA ascending aorta; aSAR anterior superior aortic recess; B bronchi; E esophagus; LA left atrium; LAA left atrial appendage; LPR left pulmonic recess; LSPV left superior pulmonary vein; MPA main pulmonary artery; OS oblique sinus; PCR postcaval recess; PPR posterior pericardial recess; pSAR posterior superior aortic recess; RA, right atrium; RAA right atrium appendage; RPA right pulmonary artery; RPR right pulmonic recess; RPVR right pulmonic vein recess; rSAR right superior aortic recess; RSPV right superior pulmonary vein; RVOT right ventricular outflow tract; SAR superior aortic recess; SVC superior vena cavaBroderick LS et al. RadioGraphics 2005;25(2):441-53. Rienmüller R et al. Radiol Clin NA 2004;42:587-601. |
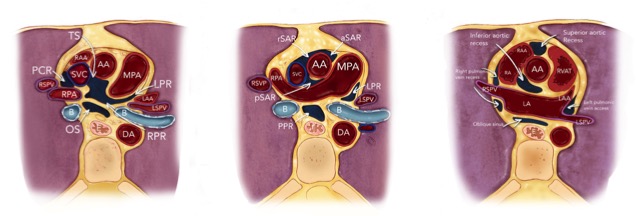
Clinical Importance of Pericardial Recesses Pericardial recess:
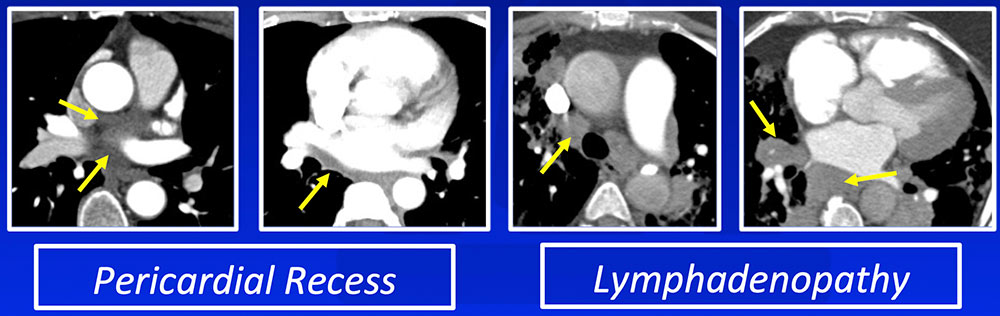 |
Multimodality Imaging in Pericardial Disease  Klein AL et al. J Am Soc Echocardiogr 2013;26:965-1012. |
Congenital Absence of the Pericardium
|
Partial Absence of the Pericardium Partial Absence of Left Pericardium:
 Wang ZJ et al. RadioGraphics 2003;23:S167-80. Cases previously published in Verde F et al. J Cardiovasc Comput Tomogr. 2013;7(1):11-7, reproduced with permission. |
Partial Absence of the Pericardium Partial Absence of Right Pericardium:
 Wang ZJ et al. RadioGraphics 2003;23:S167-80. Cases previously published in Verde F et al. J Cardiovasc Comput Tomogr. 2013;7(1):11-7, reproduced with permission. |
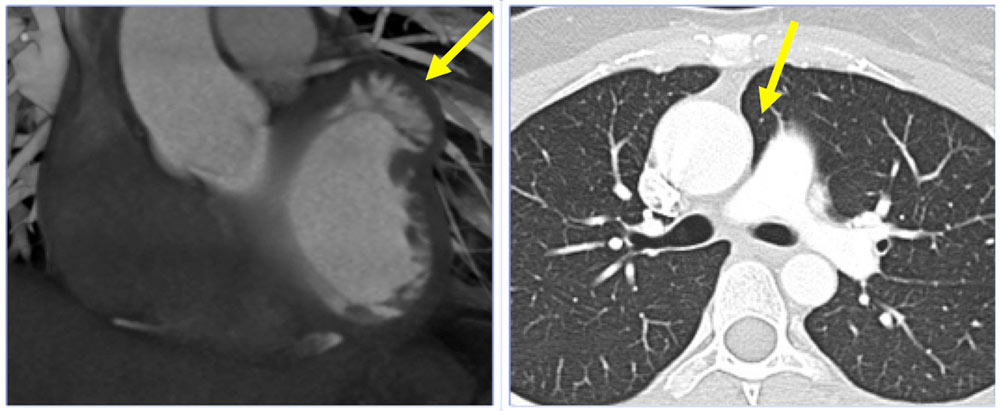
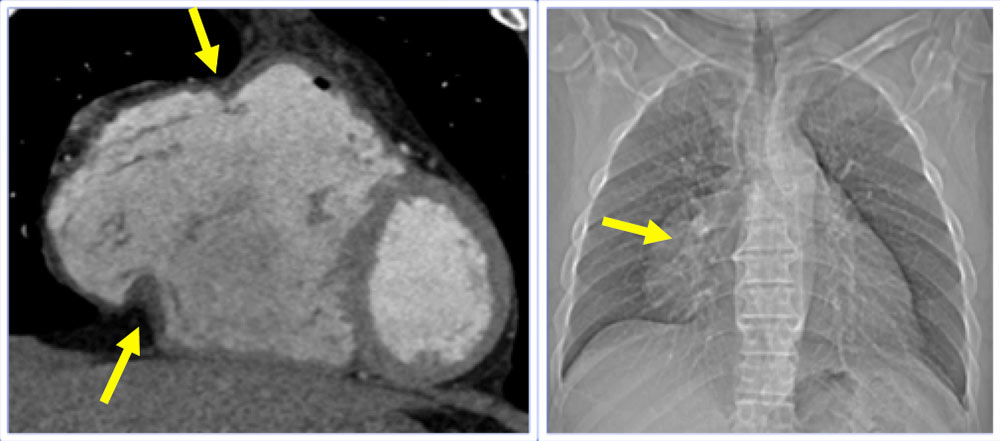
Pericardial Effusion CXR:
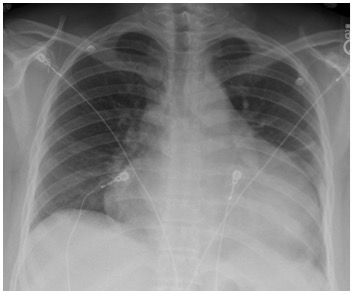 |
Transudative Pericardial Effusion
 Cummings KW et al. Semin Ultrasound CT MRI 2016;37:238-54. Rajiah P et al. J Cardiovasc Comput Tomogr 2010:4:3-18. |
Exudative Pericardial Effusion
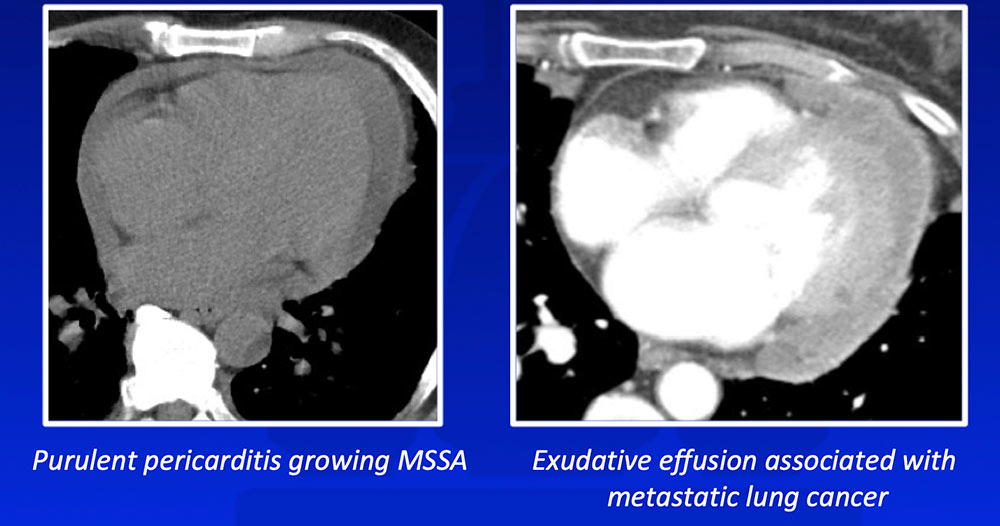 Cummings KW et al. Semin Ultrasound CT MRI 2016;37:238-54. Rajiah P et al. J Cardiovasc Comput Tomogr 2010:4:3-18. |
Hemopericardium
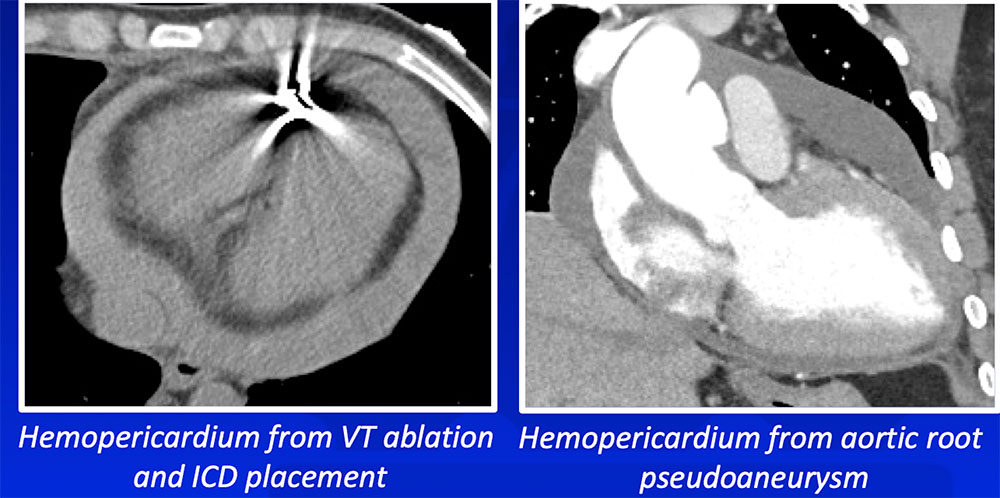 Cummings KW et al. Semin Ultrasound CT MRI 2016;37:238-54. Rajiah P et al. J Cardiovasc Comput Tomogr 2010:4:3-18. |
Pneumopericardium
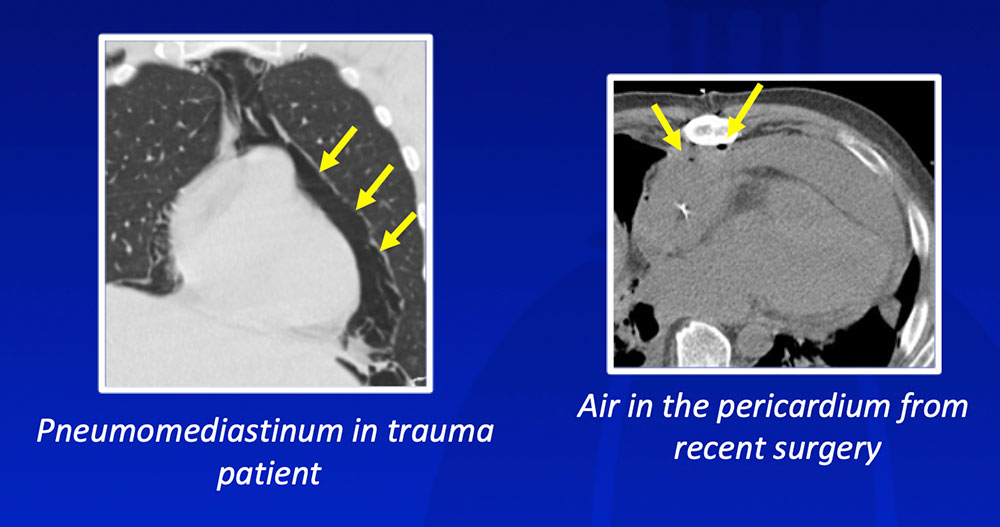 Cummings KW et al. Semin Ultrasound CT MRI 2016;37:238-54. |
Cardiac Tamponade - Pathophysiology 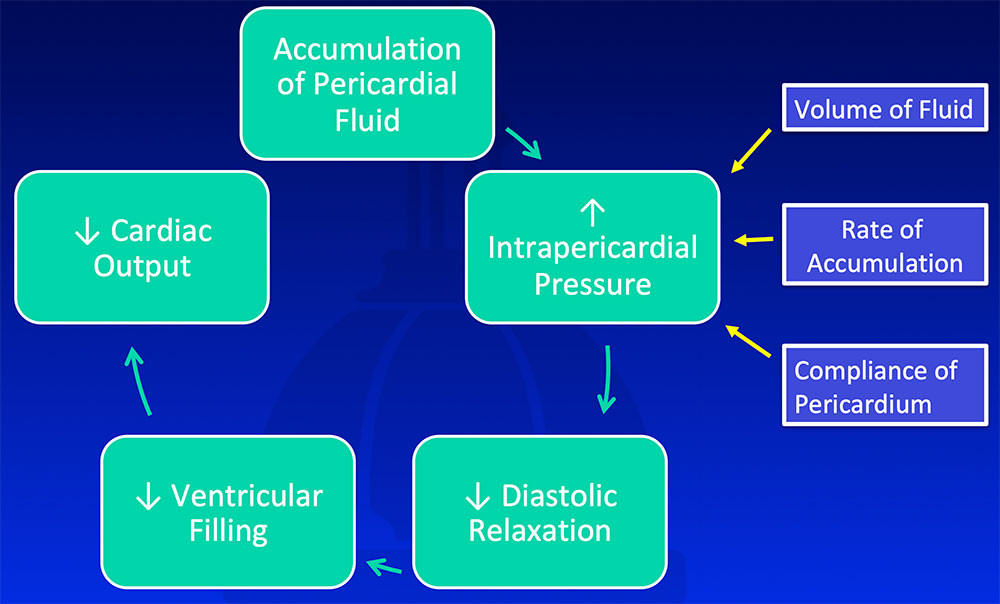 Cummings KW et al. Semin Ultrasound CT MRI 2016;37:238-54. Klein AL et al. J Am Soc Echocardiogr 2013;26:965-1012. |
Imaging Findings of Cardiac Tamponade
Klein AL et al. J Am Soc Echocardiogr 2013;26:965-1012. |
Diastolic Collapse of RA and RV ↑ Intrapericardial pressure → Diastolic collapse of RA and RV 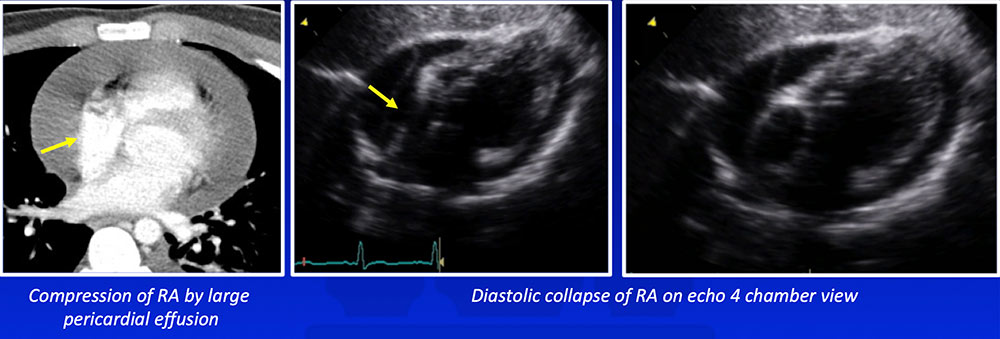 Cummings KW et al. Semin Ultrasound CT MRI 2016;37:238-54. Klein AL et al. J Am Soc Echocardiogr 2013;26:965-1012. |
Diastolic Collapse of RA and RV 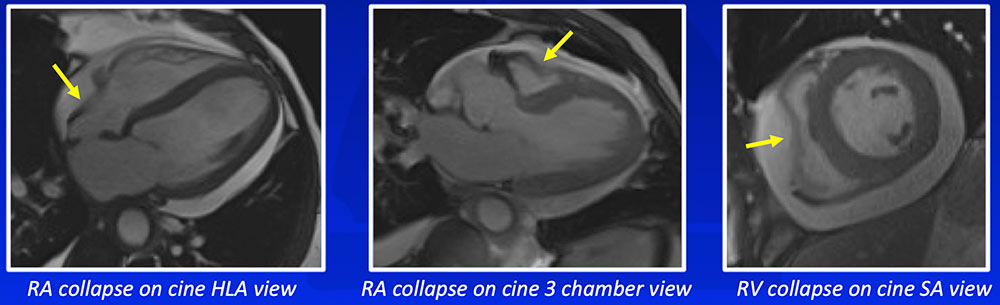 |
Septal Bowing and Reflux into IVC/Hepatic Veins
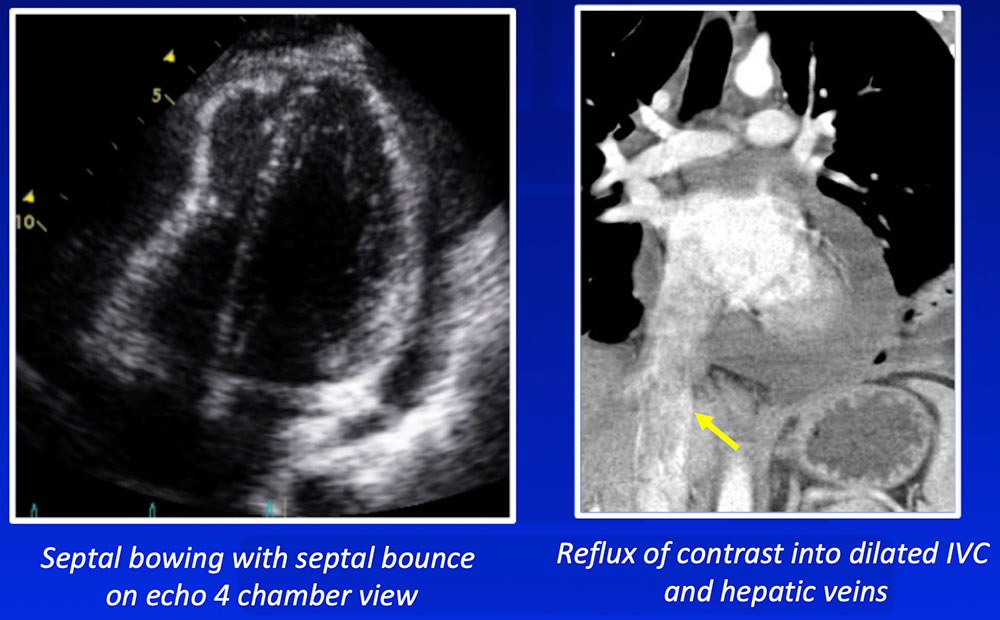 |
Acute Pericarditis
Rajiah P et al. J Cardiovasc Comput Tomogr 2010:4:3-18. |
Acute Pericarditis 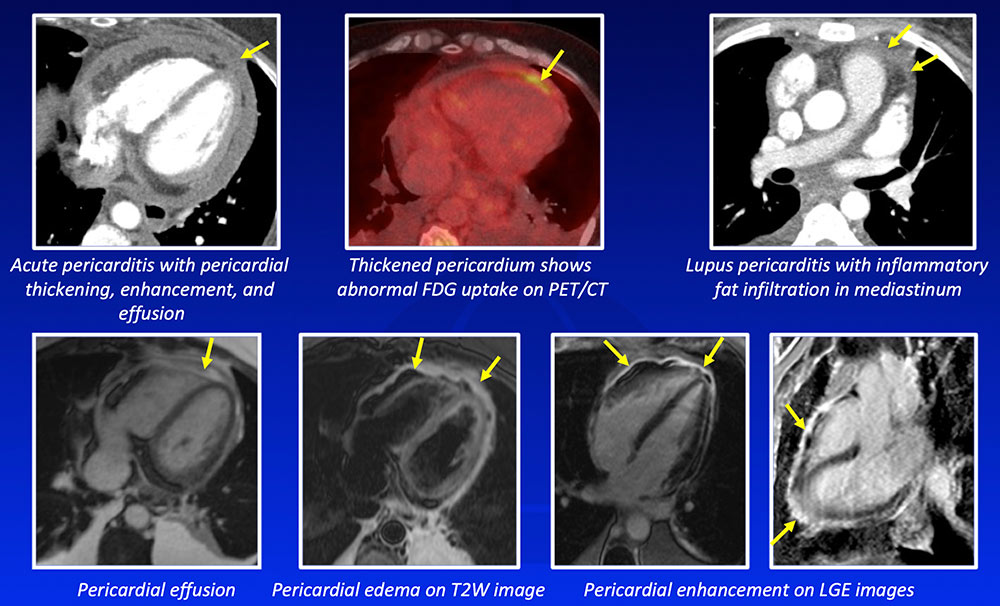 |
Constrictive Pericarditis 
Klein AL et al. J Am Soc Echocardiogr 2013;26:965-1012. Bogaert J et al. Radiology 2013;267:340-56. |
Chronic Calcific Pericarditis
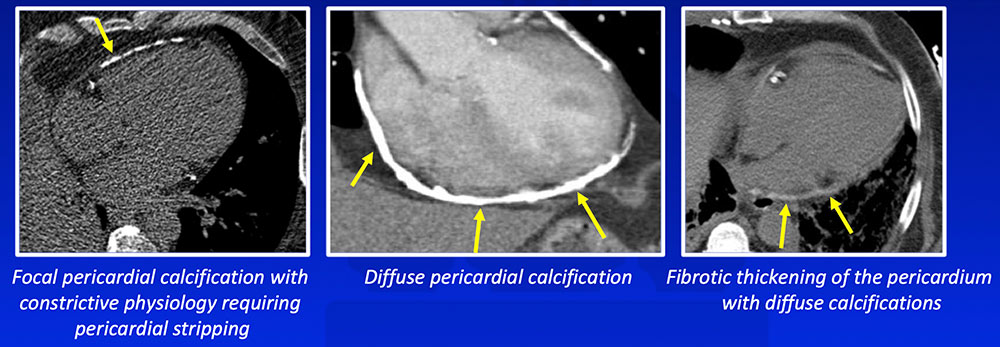 Case previously published in Chu LC et al. AJR 2014;203:W583-95, reproduced with permission. Rajiah P et al. J Cardiovasc Comput Tomogr 2010:4:3-18. |
Morphologic Features of Constrictive Pericarditis
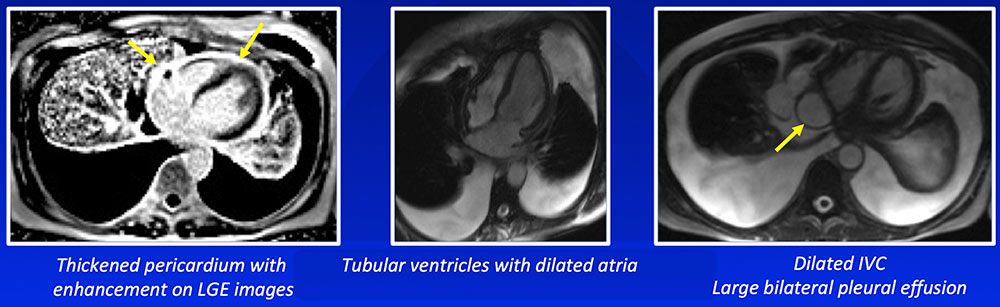 Cummings KW et al. Semin Ultrasound CT MRI 2016;37:238-54 |
Ventricular Interdependence
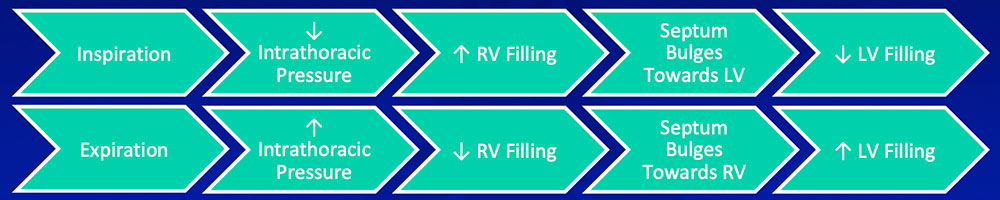 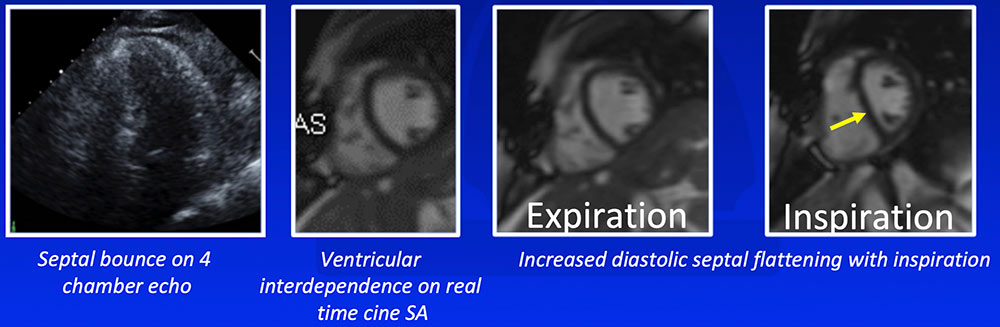 |
Pericardial-Myocardial Adherence
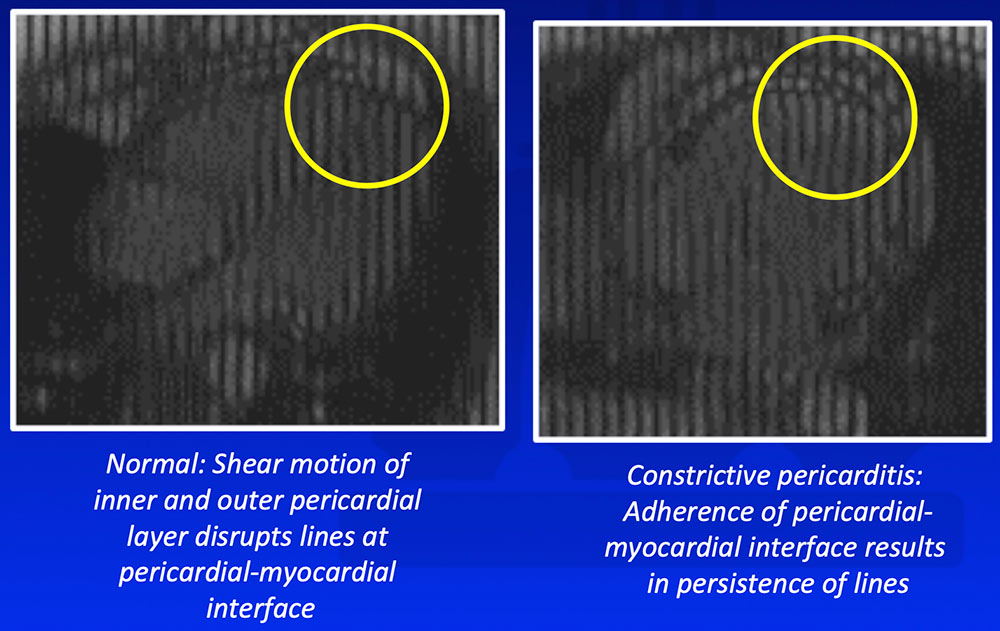 |
DDX: Restrictive Cardiomyopathy Clinical presentation similar between constrictive pericarditis and restrictive cardiomyopathy 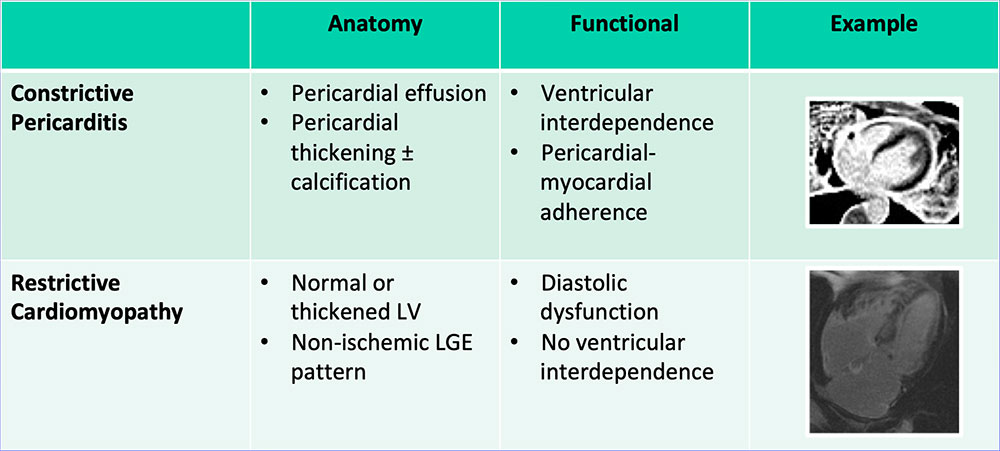 |
DDX of Pericardial Masses Key imaging features in DDX of pericardial masses:
|
Pericardial Cyst
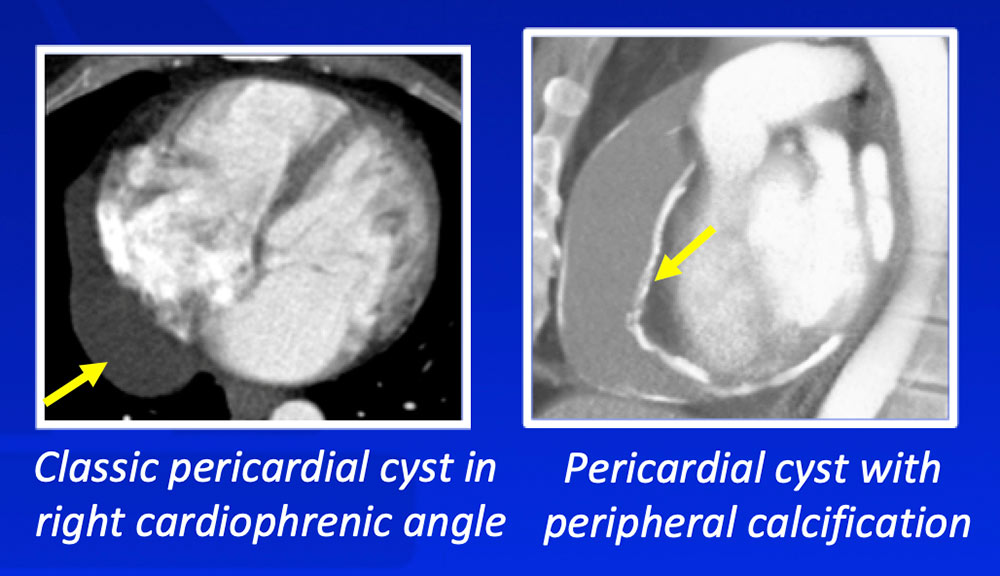 Rajiah P et al. J Cardiovasc Comput Tomogr 2010:4:3-18. |
Pericardial Hematoma
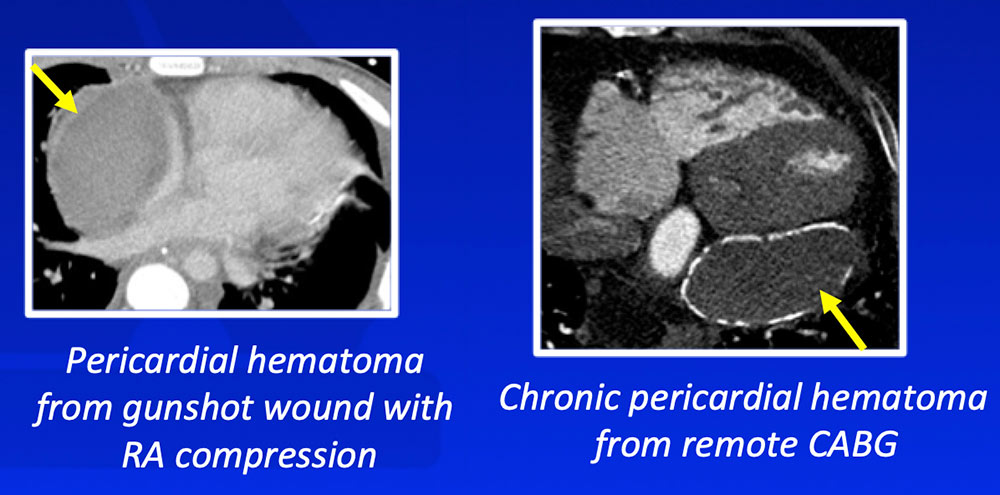 |
Pericardial Lipomatous Hypertrophy and Pericardial Lipoma Pericardial lipomatous hypertrophy:
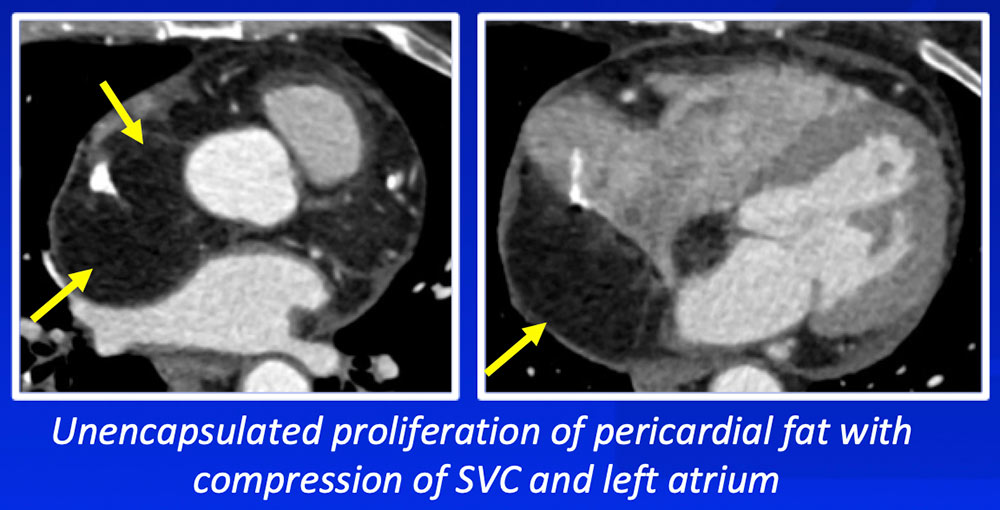 |
Pericardial Lipomatous Hypertrophy and Pericardial Lipoma Pericardial lipoma:
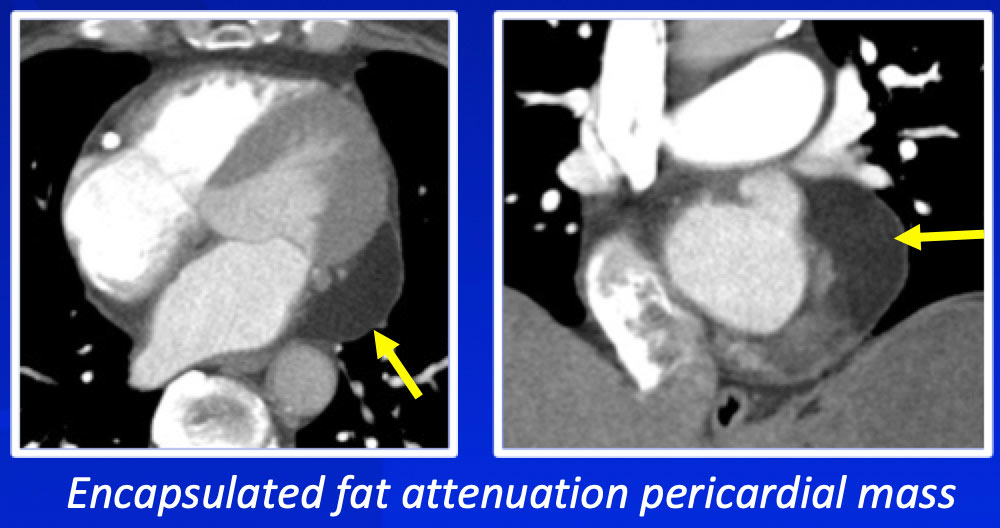 |
Malignant Pericardial Tumors Pericardial lipoma:
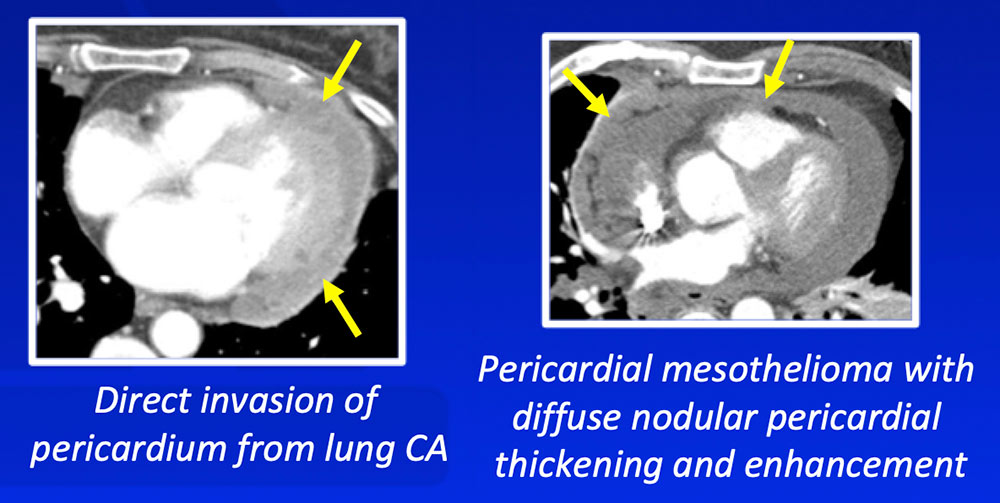 Cummings KW et al. Semin Ultrasound CT MRI 2016;37:238-54. |
Pericardial Sarcomas
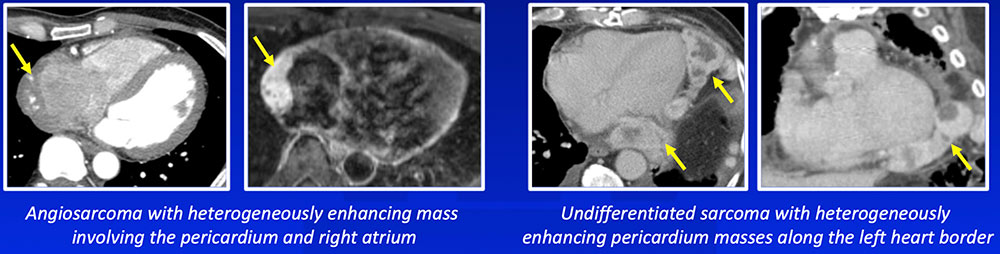 Cases previously published in Chu LC et al. Emerg Radiol 2012;19(5):415-28, reproduced with permission. |
Pericardial Lymphoma
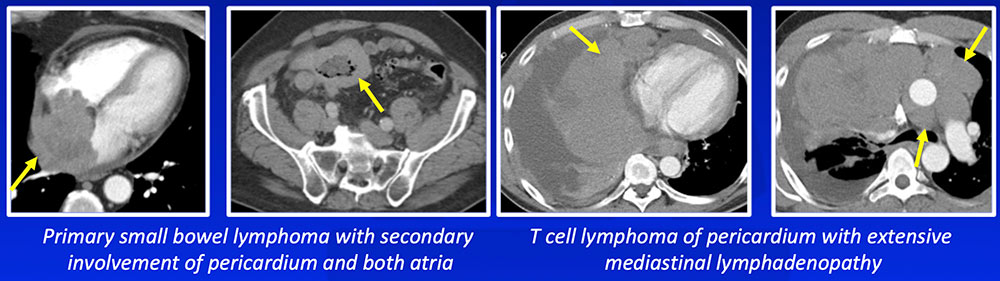 Cases previously published in Chu LC et al. Emerg Radiol 2012;19(5):415-28, reproduced with permission. |
Summary
|
References
Acknowledgements
|
