Imaging Pearls ❯ Vascular ❯ COVID-19
|
-- OR -- |
|
- “Thromboembolic complications in COVID-19 disease are likely multifactorial in etiology. However, it is believed to be in- duced by profound inflammation characterized by exaggerated re- lease of inflammatory cytokines (cytokine storm). This exaggerated inflammatory response is also known to promote thrombosis by 91%.in the assessment of patients with complications associated with COVID-19 disease, along with clinical assessment and pertinent laboratory tests, including RT-PCR. Radiologic imaging studies play an important role altering fibrinolysis and natural anticoagulant pathways. The hypercoagulable state in this disease has been aptly named COVID-19–associated coagulopathy. Patients who have severe disease have a higher prevalence of thrombotic complication; however, patients who do not have severe disease may also be at risk”
Cross-sectional Imaging Manifestations of Extrapulmonary Involvement in COVID-19 Disease
Bernard F. Laya et al.
(J Comput Assist Tomogr 2021;45: 253–262) 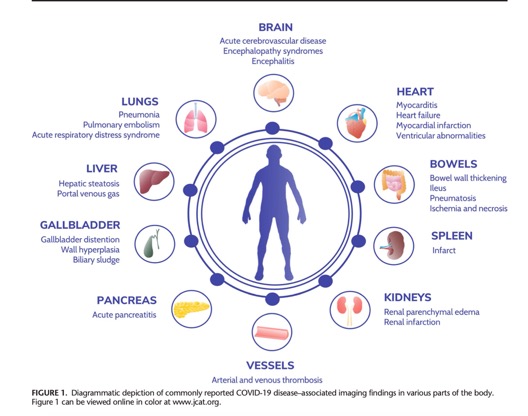
Cross-sectional Imaging Manifestations of Extrapulmonary Involvement in COVID-19 Disease
Bernard F. Laya et al.
(J Comput Assist Tomogr 2021;45: 253–262)- “Cardiac involvement in COVID-19 disease may be a primary consequence of direct invasion of the myocardium. However, it can also be secondary to a hyperinflammatory state, which can predispose atherosclerotic plaques to rupture. Consequently, the endothelial dysfunction and increased procoagulant activity of the blood raise the risk for thromboembolism. It is also important to note that as many as 40% of hospitalized patients with COVID-19 disease have preexisting CVD, which could worsen during the course of critical illness.”
Cross-sectional Imaging Manifestations of Extrapulmonary Involvement in COVID-19 Disease
Bernard F. Laya et al.
(J Comput Assist Tomogr 2021;45: 253–262) - “The spectrum of bowel cross-sectional imaging manifestations on COVID-19 patients during their hospital confinement ranges from inflammation to ischemia and necrosis. Specific findings include ileus, bowel wall thickening, altered bowel wall enhancement, pneumatosis, and portal venous gas In critically ill patients, fluid-filled colon indicative of diarrhea, as well as cholestasis, was commonly noted.”
Cross-sectional Imaging Manifestations of Extrapulmonary Involvement in COVID-19 Disease
Bernard F. Laya et al.
(J Comput Assist Tomogr 2021;45: 253–262) - “It is postulated that at least 10% of affected patients have abnormal renal function, in which the virus affects renal cells, specifically renal tubular cells. Renal cell damage could cause smalltubule atrophy, renal interstitial fibrosis, and acute kidney injury that are strongly associated with increased mortality and morbidity. Computed tomography imaging findings include inflammation and edema of the renal parenchyma, showing lower CT attenuation compared with normal. In addition multiple wedge shaped kidney defects compatible with infarctions may also be seen..”
Cross-sectional Imaging Manifestations of Extrapulmonary Involvement in COVID-19 Disease
Bernard F. Laya et al.
(J Comput Assist Tomogr 2021;45: 253–262) - "Coronavirus disease 2019 disease caused by SARS-CoV-2 virus infection is a novel disease and knowledge about its pathophysiology and manifestations continue to evolve. Although the respiratory tract is the primary system involved, extrapulmonary organ systems including cardiovascular, GI, urinary, and central nervous systems also show COVID-19–associated manifestations. It is important for both clinicians and radiologists to be familiar with these associated extrapulmonary findings to aid in early recognition and appropriate management of this disease.”
Cross-sectional Imaging Manifestations of Extrapulmonary Involvement in COVID-19 Disease
Bernard F. Laya et al.
(J Comput Assist Tomogr 2021;45: 253–262)
