Imaging Pearls ❯ Stomach ❯ Carcinoid Tumors
|
-- OR -- |
|
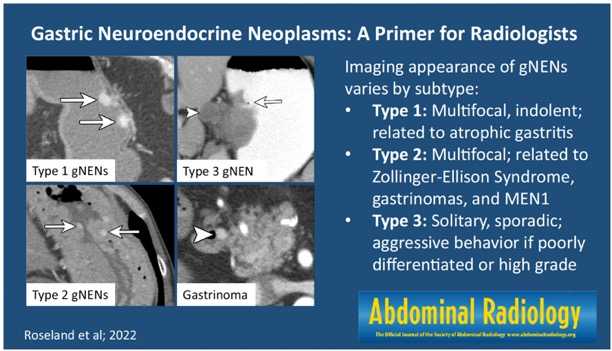
- “Gastric neuroendocrine neoplasms are uncommon tumors with variable differentiation and malignant potential. Three main subtypes are recognized: type 1, related to autoimmune atrophic gastritis; type 2, associated with Zollinger–Ellison and MEN1 syndrome; and type 3, sporadic. Although endoscopy alone is often sufficient for diagnosis and management of small, indolent, multifocal type 1 tumors, imaging is essential for evaluation of larger, high-grade, and type 2 and 3 neoplasms. Hypervascular intraluminal gastric masses are typically seen on CT/MRI, with associated perigastric lymphadenopathy and liver metastases in advanced cases. Somatostatin receptor nuclear imaging (such as Ga-68-DOTATATE PET/CT) may also be used for staging and assessing candidacy for peptide receptor radionuclide therapy.”
Gastric neuroendocrine neoplasms: a primer for radiologists
Molly E. Roseland et al.
Abdominal Radiology (2022) 47:3993–4004 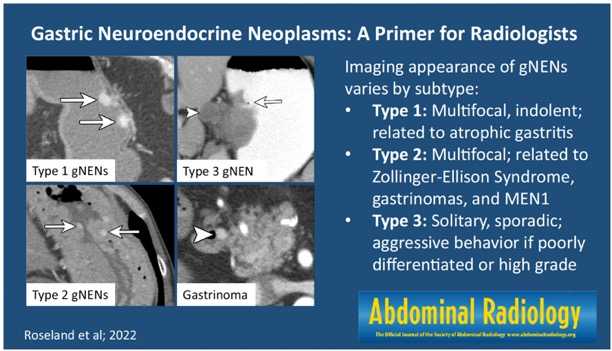
Gastric neuroendocrine neoplasms: a primer for radiologists
Molly E. Roseland et al.
Abdominal Radiology (2022) 47:3993–4004- “Gastric NENs constitute less than 2% of all gastric cancers and only 6–10% of GI tract NENs in the United States. Incidence has increased up to 15-fold since the 1970s, attributed primarily to the widespread use of endoscopy. Tumors are often detected incidentally, at early stages, with approximately 70% of patients initially presenting with localized disease. Outcomes are relatively favorable, with a 5-year disease-specific survival of 71%.”
Gastric neuroendocrine neoplasms: a primer for radiologists
Molly E. Roseland et al.
Abdominal Radiology (2022) 47:3993–4004 - “The World Health Organization (WHO) revised official pathologic definitions of GI tumors in 2019 . GI NENs are currently divided into two primary categories: well-differentiated neuroendocrine tumors (NETs) and poorly differentiated neuroendocrine carcinomas (NECs). (Note that “carcinoid” is not a formal category and has not been included in WHO terminology since the 2000 update.) Differentiation is determined by tumor histology. Well-differentiated tumors have circumscribed margins, typical morphology/ architecture, and secretory vesicles (evidenced by uniform staining for chromogranin or synaptophysin). Conversely, poorly differentiated tumors have infiltrative margins, necrosis, and “small-cell” or “large-cell” morphology.”
Gastric neuroendocrine neoplasms: a primer for radiologists
Molly E. Roseland et al.
Abdominal Radiology (2022) 47:3993–4004 - “Contrast-enhanced, multiphasic abdominal CT is the most common non-invasive modality used for primary tumor assessment and staging. It is affordable, accessible, reproducible, and familiar to clinicians, offering high spatial and temporal resolution. Exams should include arterial and venous phases with thin slices (< 1 mm with 2–3 mm multiplanar reformats) for improved visualization and precise measurement of enhancing primary tumors and any metastases. Water or neutral oral contrast (rather than dense barium) should be used, and a portion of the contrast should be administered shortly before scanning for optimal distension of the stomach and duodenum. CT most clearly depicts the perigastric and mesenteric vasculature, but is inferior to MRI for liver lesion characterization and detection of bone metastases.”
Gastric neuroendocrine neoplasms: a primer for radiologists
Molly E. Roseland et al.
Abdominal Radiology (2022) 47:3993–4004 - Type 1 tumors are the most common type of gNEN, comprising approximately 75–80% of new diagnoses, most often in women over 60 years old .These tumors arise in the setting of chronic autoimmune atrophic gastritis, a condition caused by the destruction of parietal cells in the gastric body and fundus, with resulting achlorhydria (impaired acid secretion). This condition is also more common in women, associated with multiple other autoimmune disorders, and is classically called “pernicious anemia” when coupled with intrinsic factor/vitamin B12 deficiency.
Gastric neuroendocrine neoplasms: a primer for radiologists
Molly E. Roseland et al.
Abdominal Radiology (2022) 47:3993–4004 - “CT/MRI will show multiple intraluminal polyps or masses (< 1–2 cm) in the gastric body/fundus, which are solid, round, and homogeneous, with arterial-phase hyperenhancement. Smaller tumors may be challenging to identify if the stomach is decompressed, and their appearance may mimic a polyposis syndrome if not already diagnosed by endoscopy. The surrounding gastric fundal mucosa may be thin and featureless, with few rugal folds (analogous to the so-called “bald fundus” seen on fluoroscopy), due to atrophic gastritis. Occasionally metastatic (enlarged, hypervascular) lymph nodes may be seen in the perigastric and gastrohepatic regions (5–10% of cases). Very rarely are liver metastases identified (2–5% of cases).”
Gastric neuroendocrine neoplasms: a primer for radiologists
Molly E. Roseland et al.
Abdominal Radiology (2022) 47:3993–4004 - Type 2 gNENs are rarer tumors (5% of cases), arising in the setting of hypergastrinemia from an existing gastrinoma, with associated Zollinger–Ellison syndrome. MEN1 syndrome is also present among 23–29% of patients . Type 2 gNENs occur equally among men and women.
Gastric neuroendocrine neoplasms: a primer for radiologists
Molly E. Roseland et al.
Abdominal Radiology (2022) 47:3993–4004 - “Gastrinomas are a type of functional NEN occurring commonly among patients with MEN1, usually found in the duodenum or pancreatic head, within the “gastrinoma triangle” (defined as the space between the junction of the common bile duct/cystic duct, the junction of the pancreatic neck/body, and the junction of the second/third portions of the duodenum). Gastrinomas cause abnormally elevated gastrin levels, which leads to excessive gastric acid secretion, low gastric pH, diffuse mucosal hypertrophy, and severe peptic ulcer disease. Persistent gastrin elevation also stimulates ECL cell hyperplasia and the formation of multifocal tumors, analogous to type 1. However, the MEN1 mutation is also surmised to play a role in tumor development, as gastric tumors are much less common (1–3%) with sporadic gastrinoma.”
Gastric neuroendocrine neoplasms: a primer for radiologists
Molly E. Roseland et al.
Abdominal Radiology (2022) 47:3993–4004 - CT/MRI shows multifocal, small, enhancing nodular masses in the gastric fundus/body ,associated with (and potentially obscured by) diffuse gastric fold thickening .Metastatic perigastric lymphadenopathy or hypervascular liver metastases are rarely present (3–12% of cases) .
Gastric neuroendocrine neoplasms: a primer for radiologists
Molly E. Roseland et al.
Abdominal Radiology (2022) 47:3993–4004 - Type 3 tumors comprise 15–20% of gNENs, occurring in the setting of normal gastrin levels. These tumors are more common in men over age 50 and more likely to be symptomatic at presentation (causing pain and anemia related to ulceration, weight loss, or rarely an atypical carcinoid-like syndrome from increased histamine release). Classically, type 3 tumors have been described as large (> 2 cm) and ulcerated, with 50% metastatic at presentation . However, new analyses have shown more variability in type 3 gNENs (likely related to differences in grades/differentiation); some small type 3 G1 tumors behave similarly to type 1, while large NECs are extremely aggressive.
Gastric neuroendocrine neoplasms: a primer for radiologists
Molly E. Roseland et al.
Abdominal Radiology (2022) 47:3993–4004 - “CT or MRI will show a nonspecific enhancing mass anywhere in the stomach (not limited to the gastric body/ fundus), which cannot be readily distinguished from other gastric malignancies (adenocarcinoma, lymphoma, GIST). Necrosis, ulceration, infiltrative growth, ill-defined margins, and serosal involvement may be present in poorly differentiated tumors. Heterogeneous, enlarged perigastric or upper abdominal metastatic lymph nodes are more frequent. Liver metastases may develop (either at presentation or during restaging) and are often hypervascular. Peritoneal surfaces and omentum should be carefully inspected for nodularity and ascites that indicate peritoneal carcinomatosis. Distant metastases (bones, lungs, brain) may occur and are best identified by dedicated chest CT and brain/spine MRI . Osseous metastases are more likely to be osteoblastic than osteolytic by CT, but appearance varies significantly.”
Gastric neuroendocrine neoplasms: a primer for radiologists
Molly E. Roseland et al.
Abdominal Radiology (2022) 47:3993–4004
- “High-resolution CT is the gold standard diagnostic imaging study for staging of gastric malignancies. Cinematic rendering creates a photorealistic evaluation using the standard high-resolution CT volumetric data set. This novel display method ofers unique possibilities for the evaluation of gastric masses. Here we present further observations of the role of cinematic rendering in the evaluation of gastric masses at a large tertiary care center. We ofer three valuable teaching points for the application of the cinematic rendering for gastric masses with several case examples for each teaching point, discuss potential limitations of cinematic rendering, and review future directions for cinematic rendering in this setting.”
Implementation of cinematic rendering of gastric masses into clinical practice: a pictorial review
Claire Brookmeyer · Steven P. Rowe · Linda C. Chu · Elliot K. Fishman
Abdom Radiol (NY) 2022 Jul 11.doi: 10.1007/s00261-022-03604-3.
- Benign gastric tumors
• Although these lesions demonstrate different histologic findings, the overlap of radiologic findings in many gastric tumors makes differentiation difficult.
• Clinical manifestations also overlap and can vary from severe abdominal pain and acute abdomen to vague signs such as weight loss and anemia.
• some gastric tumors cause diagnostic confusion, which may result in unnecessary surgery or inappropriate follow-up.
• some unusual gastric tumors have characteristic radiologic features that may suggest a specific diagnosis. - Lipoma
• Benign submucosal tumor composed of mature adipose tissue.
• 2%–3% of benign gastric tumors
• Usually detected incidentally.
• Large lipomas may have ulcerations as a result of pressure necrosis of the overlying mucosa and cause gastrointestinal bleeding.
• Can cause intussusception or bowel obstruction.
• Tend to occur as solitary lesions
• Most frequently in the gastric antrum - Gastric Duplications
• 7% of gastrointestinal tract duplications.
• Most are noncommunicating, spheric or ovoid closed cysts, and the most common site is the greater curvature
• The mucosal lining is usually gastric, but pseudostratified respiratory epithelium and pancreatic tissue have been found
• The clinical picture depends on their size and location as well as the presence of communication with the rest of the alimentary tract.
• Most duplications are discovered in infants. Vomiting and abdominal pain are the predominant clinical findings, although patients are frequently asymptomatic.
• US and CT show a well-defined cystic mass lying close to the greater curvature of the stomach. The presence of an echogenic inner rim and hypoechoic outer muscle layers is highly suggestive of a duplication - Leiomyoma
• Mesenchymal tumors of the gastrointestinal tract are usually incidentally discovered as a firm, protruding submucosal lesion during upper gastrointestinal examinations for unrelated conditions
• The larger tumors may occasionally cause bleeding
• Pathologically, most of these tumors are composed of spindle cells and display smooth muscle differentiation.
• Gastric mesenchymal tumors are classified immunohistochemically as leiomyomas or GISTs
• In particular, the leiomyomas are defined as being desmin positive and c-kit (CD117) negative tumors and the GISTs are defined as being c-kit positive tumors. - Schwannoma
• Neurogenic tumors of the stomach are rare
• Approximately 4% of all benign gastric tumors
• The majority of these tumors are schwannomas
• Included in the smaller group of gastrointestinal mesenchymal tumors, which contains relatively well-differentiated tumors that are identical to those arising from the somatic soft tissue
• Usually appear as discrete submucosal masses that are indistinguishable from other mesenchymal tumors
• As they outgrow their blood supply, these lesions may undergo central necrosis and ulceration.
• Schwannomas and gastrointestinal stromal tumors that show differentiation toward neural elements are histologically different tumors, although the relation between them is not clear - Glomus Tumor
• The most common benign vascular tumors of the stomach
• Typically originate from glomus bodies, which are specialized arteriovenous communications that regulate skin temperature.
• Usually occur in the gastric antrum
• Typically single tumors
• The majority of affected patients are asymptomatic
larger lesions are likely to be ulcerated and may cause upper gastrointestinal bleeding.
• At radiology, these tumors appear as smooth submucosal masses with or without ulceration
• Occasionally, may contain tiny flecks of calcification
• Enhance strongly on early-phase - Heterotopic pancreas
• The incidence in autopsies ranges 0.5%-13.7
• more common at the age of 30-50 years with a male predominance
• The usual location is in the stomach in 25%-38% of the cases, duodenum in 17%-36%, jejunum in 15%-21.7% and rare in the esophagus, gallbladder, common bile duct, spleen, mesentery, mediastinum and fallopian tubes.
• Gastric lesions are discovered in the antrum in 85%-95%, either on the posterior or anterior wall, being more common along the greater curvature.
• CT usually non specific may demonstrate the lesion which enhances similarly with the normal pancreatic tissue - “Gastric lipoma is a rare lesion, ac- counting for only 5% of gastrointestinal tract lipomas and fewer than 1% of all gastric tumors. Most gastric lipomas are small asymptomatic lesions that are detected as incidental findings at autopsy. The tumor is composed of well- differentiated adipose tissue surrounded by a fibrous capsule. Most gastric lipomas are found in the submucosa, and most are located in the pyloric antrum.”
Imaging Characteristics of Gastric Lipomas in 16 Adult and Pediatric Patients Thompson WM et al. AJR 2003;181:981–985 - “When the tumors are large (> 3–4 cm), the most common clinical presentation is upper gastrointestinal hemorrhage, either chronic or acute, caused by ulceration of the neoplasm. Abdominal pain and ob- structive symptoms are also common, especially if there is endoluminal growth that could cause intussusception.”
Imaging Characteristics of Gastric Lipomas in 16 Adult and Pediatric Patients Thompson WM et al. AJR 2003;181:981–985 - “Gastric lipomas larger than 3 cm are usually symptomatic. The most common findings pre-viously reported in the literature —obstruction and gastrointestinal bleeding—were found in our series. In our 16 patients, abdominal pain was the most common symptom (eight patients, 50%), with gastrointestinal bleeding present in six patients (38%). In two patients (13%) with no abdominal symptoms,
the gastric lipomas were discovered incidentally on imaging studies performed for reasons other than upper gastrointestinal symptoms, an occurrence that is not rare in patients with gastric lipomas.”
Imaging Characteristics of Gastric Lipomas in 16 Adult and Pediatric Patients Thompson WM et al. AJR 2003;181:981–985 - “In conclusion, our review of data for 16 patients with proven gastric lipomas revealed two significant findings. First, on upper gastrointestinal examinations, lipomas have the appearance of any submucosal tumor; they are indistinguishable from gastrointestinal stroma tumors or lymphoma. Second, CT findings are specific for the diagnosis of gastric lipoma. CT should be used to characterize large submucosal masses before endoscopic biopsy is performed.”
Imaging Characteristics of Gastric Lipomas in 16 Adult and Pediatric Patients Thompson WM et al. AJR 2003;181:981–985
- Carcinoid Tumor: Facts
- Gastric carcinoids are rare and make up less than 2% of gastric neoplasms
- GI carcinoids most common in small bowel, followed by the rectum, appendix and stomach
- Majority of gastric carcinoids have atrophic metaplastic autoimmune gastritis with or without pernicious anemia - Carcinoid Tumor: Facts
- 5-10% of gastric carcinoids are caused by hypergastrinemia from a gastrin producing tumor in association with MEN type 1.
- Approximately 30% of MEN1 patients have a gastric carcinoid tumor
- May be solitary or multiple gastric lesions
- Usually hypervascular on CT - Carcinoid Tumor: Facts
- Patients with type 2 gastric carcinoids have symptoms of ZE syndrome, with abdominal pain or bleeding from multiple ulcers, diarrhea and elevated serum gastrin levels
“ Carcinoid tumors of the gastrointestinal tract are a biologically heterogeneous group of tumors with a spectrum ranging from benign indolent tumors to aggressive metastatic malignancies.”
Imaging Features of Carcinoid Tumors of the Gastrointestinal Tract
Ganeshan D et al.
AJR 2013; 201:773-786 - Carcinoid Tumors: Clinical Presentation
- Incidental finding on CT or endoscopy
- Carcinoid syndrome
- Bowel obstruction
- Perforation
- Intussusception
- Bowel ischemia
- GI Bleeding
- Fact: symptoms will vary depending on site of primary (i.e. vomiting common in gastric carcinoid and rectal pain and bleeding in colonic carcinoids) - Gastric Carcinoid Tumors: Facts
- 12% of GI Carcinoid (NETS) tumors
- Four types of tumor with type 1 most common (70-80%) and seen in middle aged woman.
- Type 1 is associated with chronic atrophic gastritis and usually in gastric fundus or body. The lesion are usually under 1 cm and submucosal in origin
- Type 2 are least common (5-10%) and is usually multicentric and small and associated with Zollinger Ellison Syndrome - Gastric Carcinoid Tumors: Facts
- Type III account for 15-25% of gastric NETs and are usually > 2 cm in size. These are more aggressive are frequently metastasize
- Type III often present as a large mass with liver metastases
- Differential dx for type III lesion is adenocarcinoma, lymphoma, and GIST tumors
- Differential dx for type I and II lesions include polyps, Kaposi’s sarcoma, metastases (melanoma and RCC), early adenocarcinoma, glomus tumors - CT of GI Carcinoid Tumors: Facts
- Metastases more common from small bowel NETs than from colonic NETs
- Tumors over 2 cm commonly metastasize and tumor over 2 cm do not usually
- Liver metastases are usually hypervascular but may be hypovascular in up to 20% of cases
- “ Carcinoid tumors of the gastrointestinal tract are a biologically heterogeneous group of tumors with a spectrum ranging from benign indolent tumors to aggressive metastatic malignancies.”
Imaging Features of Carcinoid Tumors of the Gastrointestinal Tract
Ganeshan D et al.
AJR 2013; 201:773-786 - Carcinoid Tumors: Clinical Presentation
- Incidental finding on CT or endoscopy
- Carcinoid syndrome
- Bowel obstruction
- Perforation
- Intussusception
- Bowel ischemia
- GI Bleeding
- Fact: symptoms will vary depending on site of primary (i.e. vomiting common in gastric carcinoid and rectal pain and bleeding in colonic carcinoids) - Gastric Carcinoid Tumors: Facts
- 12% of GI Carcinoid (NETS) tumors
- Four types of tumor with type 1 most common (70-80%) and seen in middle aged woman.
- Type 1 is associated with chronic atrophic gastritis and usually in gastric fundus or body. The lesion are usually under 1 cm and submucosal in origin
- Type 2 are least common (5-10%) and is usually multicentric and small and associated with Zollinger Ellison Syndrome - Gastric Carcinoid Tumors: Facts
- Type III account for 15-25% of gastric NETs and are usually > 2 cm in size. These are more aggressive are frequently metastasize
- Type III often present as a large mass with liver metastases
- Differential dx for type III lesion is adenocarcinoma, lymphoma, and GIST tumors
- Differential dx for type I and II lesions include polyps, Kaposi’s sarcoma, metastases (melanoma and RCC), early adenocarcinoma, glomus tumors - CT of GI Carcinoid Tumors: Facts
- Metastases more common from small bowel NETs than from colonic NETs
- Tumors over 2 cm commonly metastasize and tumor over 2 cm do not usually
- Liver metastases are usually hypervascular but may be hypovascular in up to 20% of cases
- Gastric Carcinoid:
Low grade malignancies
Can metastasize
Treatment
- Treatment of hypergastrinemia
- Endoscopic excision
- Surgical resection
- Endoscopic surveillance - CT Findings
- Submucosal mass or masses
- Usually 1-4 cm
- Can mimic gastric polyps
- May have associated gastric fold thickening due to elevated gastrin levels.
- Gastric Carcinoid
- Originate from Kulchitsky cells in the crypts of Lieberkuhn
- Cytoplasm contains eosinophilic granules that have an affinity for solver stain (argenaffinomas)
- < 35% of GI carcinoids are located in stomach
- Most are in distal antrum - Gastric Carcinoid
Rare but recognized complication of prolonged severe hypergastrinemia
chronic atrophic gastritis gastrinoma - Multiple Gastric Tumors: Differential Diagnosis
- Carcinoid tumor
- Hyperplastic polyps (75% of cases)
- Adenomatous polyps Peutz-Jeghers syndrome
- Multiple hamartoma syndrome (Cowden disease)
Multiple Gastric Carcinoids
wang E, Sagel SS, Brunt EM
RadioGraphics 2009;29:1206-1209 - Types
- Type I: most common and associated with hypergastrinemia, chronic atrophic gastritis with or without pernicious anemia (70-75%)
- Type II: least common and associated with gastrin producing tumor of pancreas or small bowel and are seen with MEN-1 or Zollinger Ellison syndrome (5-10%)
- Type III: not associated with hypergastrinemia and make up 13% of cases
- Facts
- Less than 1% of gastric tumors
- 8.7% of GI carcinoid tumors
- Three types including type II which is associated with MEN-I or Zollinger-Ellison syndrome
- Can present as small <1cm polyps or diffuse gastric wall thickening - Gastric Carcinoid
- Originate from Kulchitsky cells in the crypts of Lieberkuhn
- Cytoplasm contains eosinophilic granules that have an affinity for solver stain (argenaffinomas)
- < 35% of GI carcinoids are located in stomach
- Most are in distal antrum - Gastric Carcinoid
- Rare but recognized complication of prolonged severe hypergastrinemia
- chronic atrophic gastritis gastrinoma
- ? H2 blockers
- Elevated gastrin levels can result in hyperplasia of ECL cells or carcinoid - Gastric Carcinoid
- CT Findings
- Submucosal mass or masses
- Usually 1-4 cm
- Can mimic gastric polyps
- May have associated gastric fold thickening due to elevated gastrin levels. - Gastric Carcinoid
- Low grade malignancies
- Can metastasize
- Treatment
- Treatment of hypergastrinemia
- Endoscopic excision
- Surgical resection
- Endoscopic surveillance
? H2 blockers