|
-- OR -- |
|
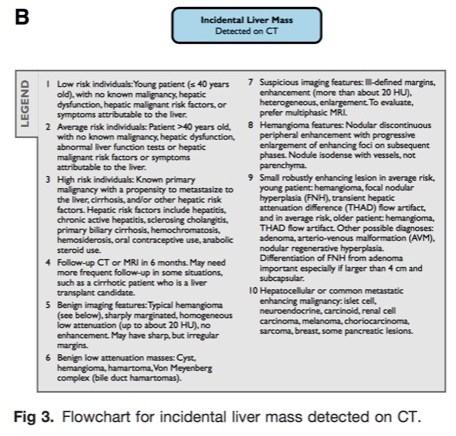
- “ Managing incidental liver lesions depends on the probable importance of the mass. Importance is assessed based on the appearance of the mass and the level of risk that each patient has for developing significant liver masses, realizing that important liver masses are not limited to malignancies. Patient risk for important hepatic masses is stratified as follows: ”
Hepatic Incidentalomas Gore RM et al. Radiol Clin North Am. 2011 Mar;49(2):291-322 - “When evaluating a small hepatic mass in the oncology patient, 2 important facts must be considered. First, at postmortem examination, benign hepatic lesions are detected in up to 52% of the general population. Second, the liver is the most common site of extranodal metastases, seen in up to 36% of patients. Small hepatic masses are commonly encountered in both populations on cross-sectional imaging. Hepatic cysts including BDHs and HHs are present in nearly 40% of patients. When less than 1.5 cm in size, these lesions can be difficult to characterize and differentiate from metastatic disease.”
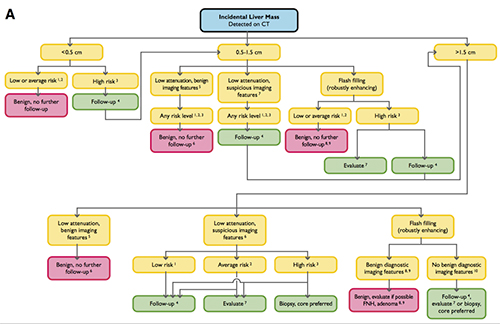
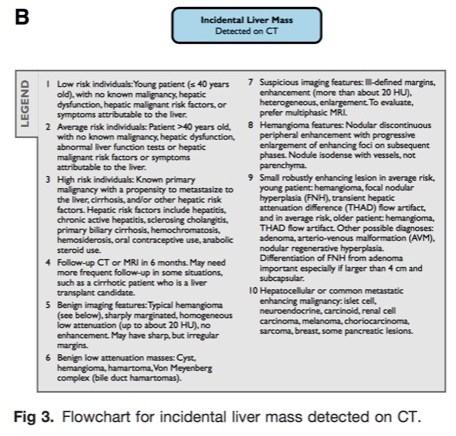
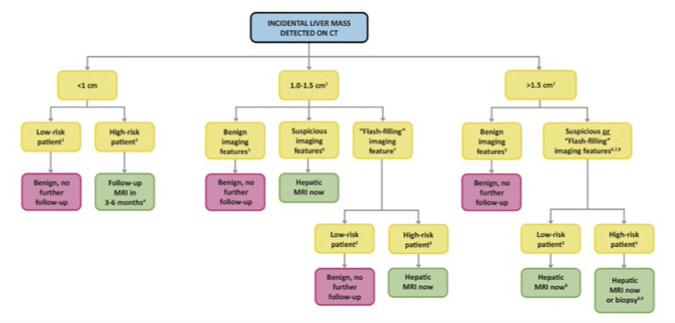
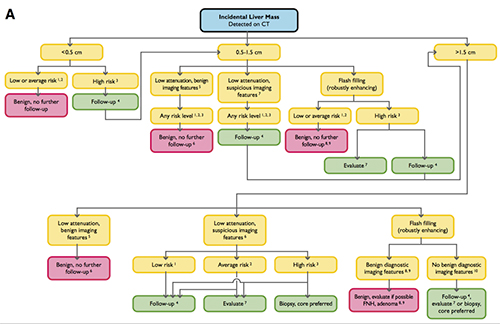
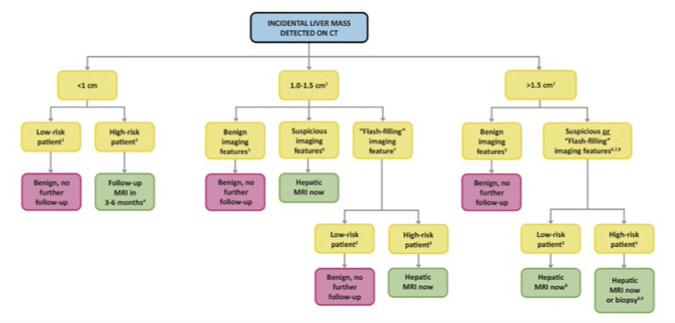
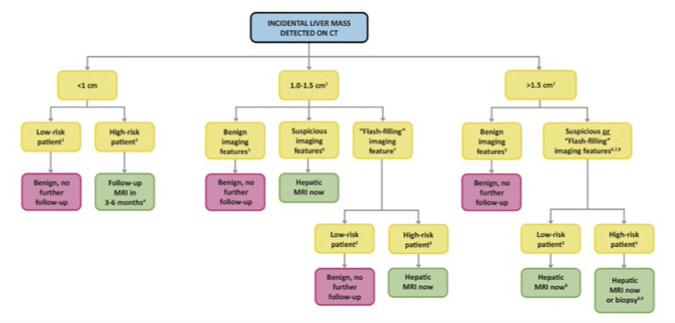
Hepatic Incidentalomas Gore RM et al. Radiol Clin North Am. 2011 Mar;49(2):291-322 - “The Incidental Findings Committee’s guidance for managing liver incidental findings is illustrated in Figure 3. Managing incidental liver lesions depends on the probable importance of the mass. This is assessed both by the appearance of the mass and the level of risk that each patient has for developing important liver masses. Important liver masses are not limited to malignancies. For example, a benign hepatic adenoma might require surgical intervention.”
Managing Incidental Findings on Abdominal CT: White Paper of the ACR Incidental Findings Committee Berland LL et al. J Am Coll Radiol 2010;7:754-773. 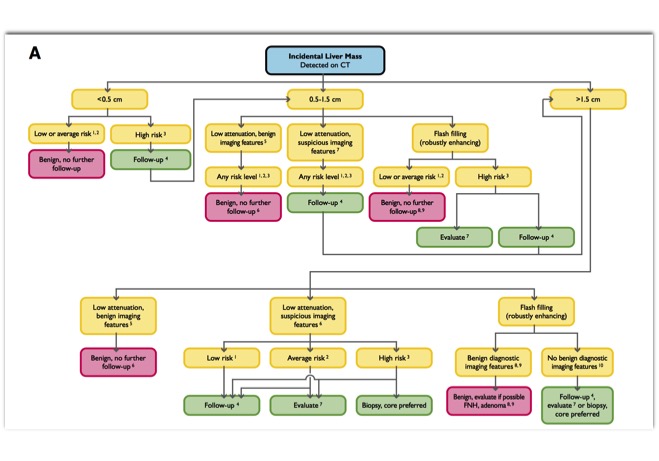
- Incidental Liver Mass Detected on CT
- “The core objectives of the Incidental Findings Project are to (1) develop consensus on patient characteristics and imaging features that are required to characterize an incidental finding, (2) provide guidance to manage such findings in ways that balance the risks and benefits to patients, (3) recommend reporting terms that reflect the level of confidence regarding a finding, and (4) focus future research by proposing a generalizable management framework across practice settings.”
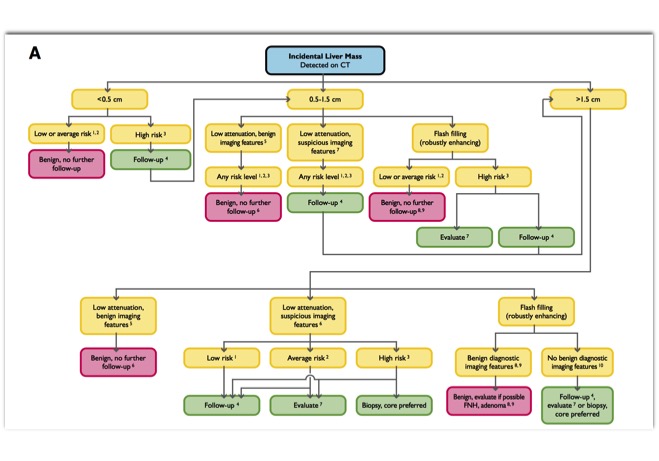
Management of Incidental Liver Lesions on CT: A White Paper of the ACR Incidental Findings Committee. Gore RM, Pickhardt PJ, Mortele KJ, Fishman EK, Horowitz JM, Fimmel CJ, Talamonti MS, Berland LL, Pandharipande PV. J Am Coll Radiol. 2017 Nov;14(11):1429-1437 - “The algorithm should only be applied to incidental liver lesions in asymptomatic adult patients (!18 years of age) for whom CT was requested for an unrelated reason. As described earlier, the algorithm is designed for use in patients with varied underlying risk levels (low versus high) for a malignant hepatic lesion. However, the algo- rithm should not be applied when index CT (i.e., that which demonstrates the incidental lesion) was requested to evaluate a known or suspected liver lesion or hepatic abnormality. There are some hepatic lesions that present with associated vascular invasion, biliary dilation, or adenopathy. Patients with these associated findings should be referred directly for oncologic evaluation.”
Management of Incidental Liver Lesions on CT: A White Paper of the ACR Incidental Findings Committee. Gore RM, Pickhardt PJ, Mortele KJ, Fishman EK, Horowitz JM, Fimmel CJ, Talamonti MS, Berland LL, Pandharipande PV. J Am Coll Radiol. 2017 Nov;14(11):1429-1437 - Reporting Considerations of a Hepatic Lesion
1. Lesion size
2. Lesion attenuation
3. Lesion homogeneity versus complexity
4. Lesion enhancement pattern
5. Lesion margin
6. Lesion multiplicity
7. Lesion growth pattern
8. Lesion location - “Specific regions of the liver are susceptible to effects of perfusional changes and fatty infiltration or sparing; such effects may mimic liver lesions . Peripherally, so-called THADs (transient hepatic attenuation differ- ences, seen on CT) and THIDs (transient hepatic intensity differences, seen on MRI) reflect changes in enhancement of the parenchyma due to relative differ- ences in hepatic arterial versus portal venous supply. Near the falciform ligament and the gallbladder fossa, alterations in venous drainage can result in focal fatty deposition or sparing.”
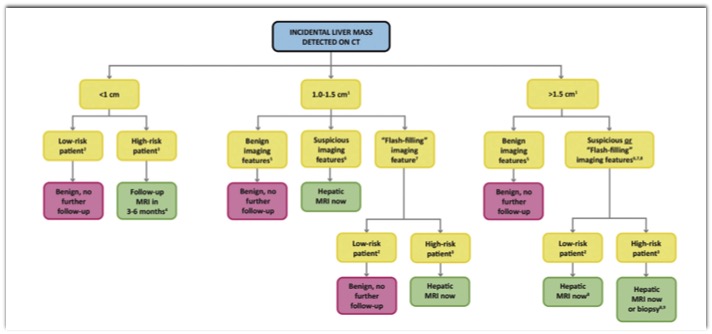
Management of Incidental Liver Lesions on CT: A White Paper of the ACR Incidental Findings Committee. Gore RM, Pickhardt PJ, Mortele KJ, Fishman EK, Horowitz JM, Fimmel CJ, Talamonti MS, Berland LL, Pandharipande PV. J Am Coll Radiol. 2017 Nov;14(11):1429-1437 - “In low-risk patients, incidental liver lesions less than 1 cm generally do not require further workup and can be considered benign. Incidental liver lesions that are 1.0 to 1.5 cm and have benign or flash-filling features also do not require further workup. Prompt MRI is advised for lesions with suspicious features that are 1.0 to 1.5 cm.”
Management of Incidental Liver Lesions on CT: A White Paper of the ACR Incidental Findings Committee. Gore RM, Pickhardt PJ, Mortele KJ, Fishman EK, Horowitz JM, Fimmel CJ, Talamonti MS, Berland LL, Pandharipande PV. J Am Coll Radiol. 2017 Nov;14(11):1429-1437 - “In high-risk patients with incidental liver lesions less than 1 cm, MRI is advised in 3 to 6 months to both characterize the lesion and document the presence or absence of growth. For lesions that are 1.0 to 1.5 cm and have benign features, no further workup with MRI is necessary; for lesions of this size with suspicious or flash-filling features, we recommend prompt MRI.”
Management of Incidental Liver Lesions on CT: A White Paper of the ACR Incidental Findings Committee. Gore RM, Pickhardt PJ, Mortele KJ, Fishman EK, Horowitz JM, Fimmel CJ, Talamonti MS, Berland LL, Pandharipande PV. J Am Coll Radiol. 2017 Nov;14(11):1429-1437 - TAKE-HOME POINTS
• Forgo workup of incidental hepatic lesions less than 1 cm in low-risk patients.
• Forgo workup of incidental hepatic lesions with distinctly benign features regardless of risk level.
• Pursue workup of incidental hepatic lesions that are over 1 cm and without distinctly benign features in high-risk patients
Management of Incidental Liver Lesions on CT: A White Paper of the ACR Incidental Findings Committee. Gore RM et al.
J Am Coll Radiol. 2017 Nov;14(11):1429-1437
Incidental Liver Mass Detected on CT
“The core objectives of the Incidental Findings Project are to (1) develop consensus on patient characteristics and imaging features that are required to characterize an incidental finding, (2) provide guidance to manage such findings in ways that balance the risks and benefits to patients, (3) recommend reporting terms that reflect the level of confidence regarding a finding, and (4) focus future research by proposing a generalizable management framework across practice settings.”
Management of Incidental Liver Lesions on CT: A White Paper of the ACR Incidental Findings Committee. Gore RM, Pickhardt PJ, Mortele KJ, Fishman EK, Horowitz JM, Fimmel CJ, Talamonti MS, Berland LL, Pandharipande PV. J Am Coll Radiol. 2017 Nov;14(11):1429-1437“The algorithm should only be applied to incidental liver lesions in asymptomatic adult patients (!18 years of age) for whom CT was requested for an unrelated reason. As described earlier, the algorithm is designed for use in patients with varied underlying risk levels (low versus high) for a malignant hepatic lesion. However, the algo- rithm should not be applied when index CT (ie, that which demonstrates the incidental lesion) was requested to evaluate a known or suspected liver lesion or hepatic abnormality. There are some hepatic lesions that present with associated vascular invasion, biliary dilation, or adenopathy. Patients with these associated findings should be referred directly for oncologic evaluation.”
Management of Incidental Liver Lesions on CT: A White Paper of the ACR Incidental Findings Committee. Gore RM, Pickhardt PJ, Mortele KJ, Fishman EK, Horowitz JM, Fimmel CJ, Talamonti MS, Berland LL, Pandharipande PV. J Am Coll Radiol. 2017 Nov;14(11):1429-1437Reporting Considerations of a Hepatic Lesion
1. Lesion size
2. Lesion attenuation
3. Lesion homogeneity versus complexity
4. Lesion enhancement pattern
5. Lesion margin
6. Lesion multiplicity
7. Lesion growth pattern
8. Lesion locationIncidental Liver Mass Detected on CT
“Specific regions of the liver are susceptible to effects of perfusional changes and fatty infiltration or sparing; such effects may mimic liver lesions . Peripherally, so-called THADs (transient hepatic attenuation differ- ences, seen on CT) and THIDs (transient hepatic intensity differences, seen on MRI) reflect changes in enhancement of the parenchyma due to relative differ- ences in hepatic arterial versus portal venous supply. Near the falciform ligament and the gallbladder fossa, alterations in venous drainage can result in focal fatty deposition or sparing.”
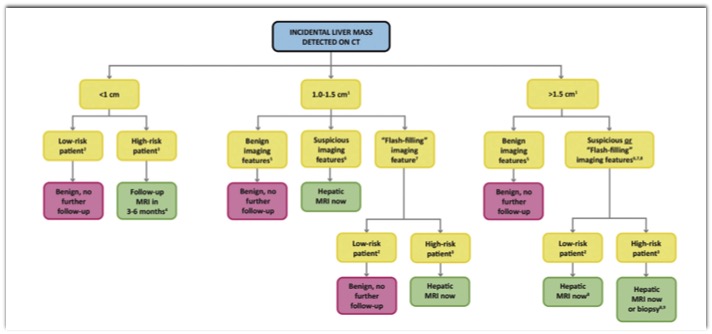
Management of Incidental Liver Lesions on CT: A White Paper of the ACR Incidental Findings Committee. Gore RM, Pickhardt PJ, Mortele KJ, Fishman EK, Horowitz JM, Fimmel CJ, Talamonti MS, Berland LL, Pandharipande PV. J Am Coll Radiol. 2017 Nov;14(11):1429-1437“In low-risk patients, incidental liver lesions less than 1 cm generally do not require further workup and can be considered benign. Incidental liver lesions that are 1.0 to 1.5 cm and have benign or flash-filling features also do not require further workup. Prompt MRI is advised for lesions with suspi- cious features that are 1.0 to 1.5 cm.”
Management of Incidental Liver Lesions on CT: A White Paper of the ACR Incidental Findings Committee. Gore RM, Pickhardt PJ, Mortele KJ, Fishman EK, Horowitz JM, Fimmel CJ, Talamonti MS, Berland LL, Pandharipande PV. J Am Coll Radiol. 2017 Nov;14(11):1429-1437“In high-risk patients with incidental liver lesions less than 1 cm, MRI is advised in 3 to 6 months to both characterize the lesion and document the presence or absence of growth. For lesions that are 1.0 to 1.5 cm and have benign features, no further workup with MRI is necessary; for lesions of this size with suspicious or flash-filling features, we recommend prompt MRI.”
Management of Incidental Liver Lesions on CT: A White Paper of the ACR Incidental Findings Committee. Gore RM, Pickhardt PJ, Mortele KJ, Fishman EK, Horowitz JM, Fimmel CJ, Talamonti MS, Berland LL, Pandharipande PV. J Am Coll Radiol. 2017 Nov;14(11):1429-1437TAKE-HOME POINTS
• Forgo workup of incidental hepatic lesions less than 1 cm in low-risk patients.
• Forgo workup of incidental hepatic lesions with distinctly benign features regardless of risk level.
• Pursue workup of incidental hepatic lesions that are over 1 cm and without distinctly benign features in high-risk patients
Management of Incidental Liver Lesions on CT: A White Paper of the ACR Incidental Findings Committee. Gore RM et al. J Am Coll Radiol. 2017 Nov;14(11):1429-1437Incidental Liver Mass Detected on CT
- “With the widespread use of medical imaging has come the detection of incidental liver lesions that are, by and large, asymptomatic prior to their discovery. These lesions may become a source of anxiety and often require further investigation to reassure the patient of their usually benign nature. Use of contemporary hepatobiliary imaging and simple laboratory tests often allow a definite diagnosis to be made without resorting to exhaustive investigation or inappropriate surgery.”
Investigation and management of hepatic incidentalomas. Fergusson J J Gastroenterol Hepatol. 2012 Dec;27(12):1772-82. - “Managing incidental liver lesions depends on the probable importance of the mass. Importance is assessed based on the appearance of the mass and the level of risk that each patient has for developing significant liver masses, realizing that important liver masses are not limited to malignancies. Patient risk for important hepatic masses is stratified as follows: ”
Hepatic Incidentalomas Gore RM et al. Radiol Clin North Am. 2011 Mar;49(2):291-322 - 1. Low-risk individuals: Young patients (≤40 years old), with no malignancy, hepatic dysfunction, hepatic malignant risk factors, or symptoms related to the liver
2. Average risk individuals: Patients older than 40 years, with no known malignancy, hepatic dysfunction, hepatic malignant risk factors, or symptoms related to the liver Hepatic Incidentalomas
Gore RM et al. Radiol Clin North Am. 2011 Mar;49(2):291-322 - 3. High-risk individuals: Patients with a known primary malignancy with a propensity to metastasize to the liver, cirrhosis, and/or other hepatic risk factor. Hepatic risk factors include cirrhosis, hepatitis, chronic active hepatitis, sclerosing cholangitis, hemosiderosis, hepatic dysfunction, and long-term anabolic steroid or oral contraceptive use.
Hepatic Incidentalomas Gore RM et al. Radiol Clin North Am. 2011 Mar;49(2):291-322 - “When evaluating a small hepatic mass in the oncology patient, 2 important facts must be considered. First, at postmortem examination, benign hepatic lesions are detected in up to 52% of the general population. Second, the liver is the most common site of extranodal metastases, seen in up to 36% of patients. Small hepatic masses are commonly encountered in both populations on cross-sectional imaging. Hepatic cysts including BDHs and HHs are present in nearly 40% of patients.When less than 1.5 cm in size, these lesions can be difficult to characterize and differentiate from metastatic disease.”
Hepatic Incidentalomas Gore RM et al. Radiol Clin North Am. 2011 Mar;49(2):291-322 - “The Incidental Findings Committee’s guidance for managing liver incidental findings is illustrated in Figure 3. Managing incidental liver lesions depends on the probable importance of the mass. This is assessed both by the appearance of the mass and the level of risk that each patient has for developing important liver masses. Important liver masses are not limited to malignancies. For example, a benign hepatic adenoma might require surgical intervention.”
Managing Incidental Findings on Abdominal CT: White Paper of the ACR Incidental Findings Committee Berland LL et al. J Am Coll Radiol 2010;7:754-773.