Imaging Pearls ❯ September 2016
|
-- OR -- |
|
3D and Workflow
- “Our results showed similarly high levels of agreement for CAD scores between our test readers and reference readers, independent of whether an iPhone or standard workstation was used. Intraobserver intertechnology agreement was higher for each test reader than their corresponding interobserver agreement with the reference reader.”
Evaluation of coronary artery disease and coronary anomalies with a handheld mobile device Cheng Ting Lin, Stefan Loy Zimmerman, Linda Chu, John Eng, Elliot K Fishman AJR (in review) - “Coronary CTA examinations can be interpreted on a smartphone with diagnostic accuracy comparable to a standard workstation. DICOM-viewing app on the iPhone may facilitate urgent coronary CTA review when a workstation is not available.”
Evaluation of coronary artery disease and coronary anomalies with a handheld mobile device Cheng Ting Lin, Stefan Loy Zimmerman, Linda Chu, John Eng, Elliot K Fishman AJR (in review)
- “We developed a physically-based volume rendering method called Cinematic Rendering which computes in real-time the interaction of visible photons with the scanned patient anatomy. The algorithm uses a Monte Carlo path tracing method to generate photorealistic or even hyper-realistic images by light transport simulation along hundreds or thousands of photons paths per pixel through the anatomy using a stochastic process.”
Shaping the future through innovations: From medical imaging to precision medicine. Comaniciu D et al. Med Image Anal. 2016 Jun 15 (in press) - “The medical data is illuminated using image-based lighting by high-dynamic range lighting environments, which can either be captured photographically or generated synthetically. Photographically captured lighting leads to a very natural appearance of the data when compared to images created using the traditional ray casting method. Such natural lighting in combination with the accurate simulation of photon scattering and absorption, leads to photorealistic images that resemble many shading effects that can be observed in nature, such as soft shadows, ambient occlusion, volumetric scattering and subsurface photon interaction.”
Shaping the future through innovations: From medical imaging to precision medicine. Comaniciu D et al. Med Image Anal. 2016 Jun 15 (in press) - “Fast and robust anatomical concept extraction is a fundamental task in medical image analysis that supports the entire workflow from diagnosis, patient stratification, therapy planning, intervention and follow-up. Current state-of-the art solutions are based on machine learning, being enabled by the availability of large annotated medical databases and the increased computational capabilities . Typical methods use example images of the anatomy of interest to learn a classifier that will be able to discriminate between inputs that contain the target anatomy or something else. Such classifiers can be used to automatically label images, detect landmarks or segment the target object.”
Shaping the future through innovations: From medical imaging to precision medicine. Comaniciu D et al. Med Image Anal. 2016 Jun 15 (in press) - “In this paper we discussed recent technologies that will most likely make an important impact on medical imaging. Techniques like Cinematic Rendering will help increasing the sensitivity and specificity of images, by enhancing the pathology conspicuity. Advanced image understanding will streamline the image measurements and image interpretation, by increasing the speed of reading, while introducing more reproducibility in the system.”
Shaping the future through innovations: From medical imaging to precision medicine. Comaniciu D et al. Med Image Anal. 2016 Jun 15 (in press)
Cardiac
- OBJECTIVE. The objective of the present study is to quantify the diagnostic yield of triple-rule-out (TRO) CT for the evaluation of acute chest pain in emergency department patients.
CONCLUSION. In 8.9% of patients, TRO CT detected a significant noncoronary diagnosis that could explain acute chest pain, including pathologic findings that would not be identified on dedicated coronary CT angiography.
Diagnostic Yield of Triple-Rule-Out CT in an Emergency Setting Amelia M. Wnorowski, Ethan J. Halpern AJR 2016; 207:295–301 - “Acute coronary syndrome (ACS) accounts for a minority of acute chest pain presentations and was diagnosed in only 13% of patients who visited the emergency department for chest pain in 2007–2008 . However, ACS is a serious cause of chest pain, with an associated mortality rate of 3–33% and high associated morbidity, because up to 30% of patients with ACS who are discharged from the emergency department are rehospitalized within 6 months.”
Diagnostic Yield of Triple-Rule-Out CT in an Emergency Setting Wnorowski AM, Halpern EJ AJR 2016; 207:295–301 - “For the diagnosis of coronary artery disease, TRO CT has a sensitivity of 94.3%, a specificity of 97.4%, and a negative predictive value of 99%, findings that are similar to those obtained with the use of dedicated coronary CTA.”
Diagnostic Yield of Triple-Rule-Out CT in an Emergency Setting Wnorowski AM, Halpern EJ AJR 2016; 207:295–301 - “Although coronary disease was the most common diagnosis that explained chest pain, accounting for chest pain in 11.7% of our emergency department patients, TRO CT identified noncoronary diagnoses that could explain the presentation in 8.9% of our patient population. Pulmonary embolism was the most commonly noted noncoronary diagnosis.”
Diagnostic Yield of Triple-Rule-Out CT in an Emergency Setting Wnorowski AM, Halpern EJ AJR 2016; 207:295–301 - “On the basis of our retrospective review of CT findings, 30 (27.3%) of the patients with significant noncoronary diagnoses (28 of whom had pulmonary embolism and two of whom had an aortic pathologic finding) would not have been identified with the use of dedi- cated coronary CTA because of unopacified right-side circulation or limited z-axis cover- age (in patients with aortic pathologic find- ings).”
Diagnostic Yield of Triple-Rule-Out CT in an Emergency Setting Wnorowski AM, Halpern EJ AJR 2016; 207:295–301 - “In our patient population, more than 80% of patients had negative study results without significant coronary or noncoronary diagnoses. This is similar to the results of a previous study, in which 76% of patients did not require further testing. In the same study, TRO CT had a negative predictive value of 99.4% and was associated with no adverse outcomes.”
Diagnostic Yield of Triple-Rule-Out CT in an Emergency Setting Wnorowski AM, Halpern EJ AJR 2016; 207:295–301 - “Our experience with close to 1200 consecutive TRO CT studies over 10 years found that TRO CT identified significant and potentially fatal noncoronary diagnoses in 8.9% of the presenting population. The frequency of these noncoronary diagnoses is dependent on an appropriately selected patient population with a low to intermediate risk of ACS and for whom alternative diagnoses should also be considered, including pulmonary embolism and acute aortic pathology. TRO CT also identifies patients at risk for ACS and allows discharge of a majority of patients with negative study results.”
Diagnostic Yield of Triple-Rule-Out CT in an Emergency Setting Wnorowski AM, Halpern EJ AJR 2016; 207:295–301
Musculoskeletal
- OBJECTIVE. The purpose of this study was to determine whether CT attenuation thresholds can be used to distinguish untreated osteoblastic metastases from enostoses.
CONCLUSION. CT attenuation measurements can be used to distinguish untreated osteoblastic metastases from enostoses. A mean attenuation of 885 HU and a maximum attenuation of 1060 HU provide reliable thresholds below which a metastatic lesion is the favored diagnosis.
Distinguishing Untreated Osteoblastic Metastases From Enostoses Using CT Attenuation Measurements Ulano A et al. AJR 2016; 207:362–368 - “The most common malignancy of bone is metastatic disease, affecting approximately 400,000 people in the United States each year. Prostate, breast, and lung cancer account for approximately 80% of skeletal metastases.”
Distinguishing Untreated Osteoblastic Metastases From Enostoses Using CT Attenuation Measurements Ulano A et al. AJR 2016; 207:362–368 - “Our study shows that a mean CT attenuation threshold of 885 HU and a maximum attenuation threshold of 1060 HU can be helpful in differentiating untreated osteoblastic metastasis from enostosis with 95% sensitivity and 96% specificity.”
Distinguishing Untreated Osteoblastic Metastases From Enostoses Using CT Attenuation Measurements Ulano A et al. AJR 2016; 207:362–368 - “An enostosis is a benign osseous lesion that consists of a focal area of mature compact (cortical) bone within the cancellous bone (spongiosa). The finding was initially described by Stieda and Fischer in the early 20th century as “compact bone nuclei” and “islands,” respectively.”
Distinguishing Untreated Osteoblastic Metastases From Enostoses Using CT Attenuation Measurements Ulano A et al. AJR 2016; 207:362–368 - “In our study, the distribution of tumors may have affected the threshold. For example, if more cases of prostate cancer had been included, the threshold may have been higher. Further investigation should also be performed to confirm these thresholds. Because prostate metastases disproportionately measured out- side the thresholds, lesions in patients with a history of prostate cancer should be interpreted with added caution.”
Distinguishing Untreated Osteoblastic Metastases From Enostoses Using CT Attenuation Measurements Ulano A et al. AJR 2016; 207:362–368
Pancreas
- “Heterotopic pancreas represents a congenital anomaly where aberrant pancreatic tissue is without ductal or vascular continuity to the gland. The reported incidence ranges from 0.55–13.7%,however, the true incidence is unknown as most patients are asymptomatic and the condition is usually an incidental finding at autopsy or laparotomy. Most ectopic pancreatic tissue is found incidentally during evaluation of other organs. Common sites of involvement include the upper portions of the gastrointestinal tract including the stomach, duodenum, and proximal jejunum.”
Heterotopic pancreas: typical and atypical imaging findings J.W. Kung et al. Clinical Radiology 65 (2010) 403–407 - “However, most individuals remain asymptomatic clinically and are detected during surgery or endoscopy for another evaluation. When symptoms do occur the majority are related to a combination of mass effect and the local and systemic complications of activated pancreatic enzymes.15 Other possible presentations include obstruction from duodenal or pyloric stricture, gastrointestinal hemorrhage, or elevation in serum amylase and lipase..”
Heterotopic pancreas: typical and atypical imaging findings J.W. Kung et al. Clinical Radiology 65 (2010) 403–407 - “Heterotopic pancreas is most often incidentally discovered in the upper gastrointestinal tract, with the stomach
being the most common location. Lesions in the stomach range from 1–3 cm and are usually located along the greater
curvature in the gastric antrum within 6cm of the pylorus.”
Heterotopic pancreas: typical and atypical imaging findings J.W. Kung et al. Clinical Radiology 65 (2010) 403–407 - “At CT a prospective diagnosis of heterotopic pancreas is challenging. Masses are often oval or round with smooth or serrated margins in the gastric antral wall. Often there is homogeneous early enhancement, similar to the normal pancreas. Occasionally, poor enhancement is seen, in which case lesions have been shown to consist primarily of ducts and hypertrophied muscle. A minority of cases show dilatation of heterotopic pancreatic duct.”
Heterotopic pancreas: typical and atypical imaging findings J.W. Kung et al. Clinical Radiology 65 (2010) 403–407
Practice Management
- “Management is about doing things right, whereas leadership is about doing the right things.”
Learning About Leadership by Making Mistakes Brody WR, Fishman EK, Horton KM, Raman SP. J Am Coll Radiol. 2016 Jul 27. - “Leadership is a vague term, but it is readily apparent to everyone when it is absent. There always comes a time when there is a true test for an organization, and you then know who is a true leader. Leadership styles range from Attila the Hun to a consensus maker like Gandhi, and each style can be successful or a failure depending on the individual environment.”
Learning About Leadership by Making Mistakes Brody WR, Fishman EK, Horton KM, Raman SP. J Am Coll Radiol. 2016 Jul 27. - “Management guru Peter Drucker once said something like “the three most charismatic leaders in the 20th century were Hitler, Stalin, and Mao. Their problem was not bad charisma, it was bad mission.” Admittedly, I don’t have the perfect answer to this dilemma, but I will say that my experiences have taught me one lesson: never hire second best. If you can’t find the optimal candidate just restart your search.”
Learning About Leadership by Making Mistakes Brody WR, Fishman EK, Horton KM, Raman SP. J Am Coll Radiol. 2016 Jul 27. - “Taking the time to listen to your people is critical, especially for someone like me, who is used to making quick decisions. Soon after taking my first leadership position, I quickly realized that I needed to be the last person who spoke at a meeting, rather than the first. An effective leader needs to hear both sides of an issue before making a proper decision.”
Learning About Leadership by Making Mistakes Brody WR, Fishman EK, Horton KM, Raman SP. J Am Coll Radiol. 2016 Jul 27. - “As a manager, you are almost al ways the last person to know about major problems, and your employees (often out of fear of conveying un- pleasant news) may not tell you about problems that can quickly snowball into larger catastrophes for your company. Listen to what your people tell you, but also try to understand their motivations to get better insights into why different people give you different information or advice.”
Learning About Leadership by Making Mistakes Brody WR, Fishman EK, Horton KM, Raman SP. J Am Coll Radiol. 2016 Jul 27. - “Just as important, the collective wisdom of crowds (or your employees) may not always be correct, and sometimes you have to “trust your gut” more than the advice you receive or even rational analysis. Listening to the people who work for you can also be critical for keeping your job! Leaders are ultimately fired not by their bosses but rather by the people below them.”
Learning About Leadership by Making Mistakes Brody WR, Fishman EK, Horton KM, Raman SP. J Am Coll Radiol. 2016 Jul 27. - “The perfect leader is a person who is needed by the company more than he or she needs the company’s job. Be willing to make unpopular decisions that might even cost you your job if that is the right thing to do.” Learning About Leadership by Making Mistakes Brody WR, Fishman EK, Horton KM, Raman SP. J Am Coll Radiol. 2016 Jul 27.
- “Having the integrity to do the right thing, no matter what the personal consequences, is what ultimately differentiates the very best of leaders.”
Learning About Leadership by Making Mistakes Brody WR, Fishman EK, Horton KM, Raman SP. J Am Coll Radiol. 2016 Jul 27.
- “Participation in the peer review process is one means by which errors in radiology diagnosis can be identified, but the effectiveness of these programs is hampered by physicians’ reluctance to implicate their colleagues in misdiagnosis. Survey data show that nonanonymized peer review increases anxiety, raises concerns over malpractice and job security, and has the potential to strain relationships with colleagues.”
Mitigating Misdiagnosis in Radiology: Educational CT CME Case Conference for Peer Review and Interpretative Improvement Pamela T. Johnson, David Badger, Karen M. Horton, Elliot K. Fishman http://dx.doi.org/10.1016/j.jacr.2016.05.015 - “The appeal is the ability to learn from challenging cases in an atmosphere that does not result in direct criticism of any individual physician. As a result, our search patterns, protocol design, and interpretative practice have been refined to avoid commonly missed diagnoses and misdiagnoses.”
Mitigating Misdiagnosis in Radiology: Educational CT CME Case Conference for Peer Review and Interpretative Improvement Pamela T. Johnson, David Badger, Karen M. Horton, Elliot K. Fishman http://dx.doi.org/10.1016/j.jacr.2016.05.015 - “The appeal is the ability to learn from challenging cases in an atmosphere that does not result in direct criticism of any individual physician. As a result, our search patterns, protocol design, and interpretative practice have been refined to avoid commonly missed diagnoses and misdiagnoses.”
Mitigating Misdiagnosis in Radiology: Educational CT CME Case Conference for Peer Review and Interpretative Improvement Pamela T. Johnson, David Badger, Karen M. Horton, Elliot K. Fishman http://dx.doi.org/10.1016/j.jacr.2016.05.015 - “A monthly CME conference with pa- thology and/or surgical correlation
and clinical follow-up is an excellent means of providing meaningful peer review to improve practice of the entire division and reduce interpretative errors.”
Mitigating Misdiagnosis in Radiology: Educational CT CME Case Conference for Peer Review and Interpretative Improvement Pamela T. Johnson, David Badger, Karen M. Horton, Elliot K. Fishman http://dx.doi.org/10.1016/j.jacr.2016.05.015
Quotes

- "To infinity... and beyond!”
Buzz Lightyear (Toy Story)
Small Bowel
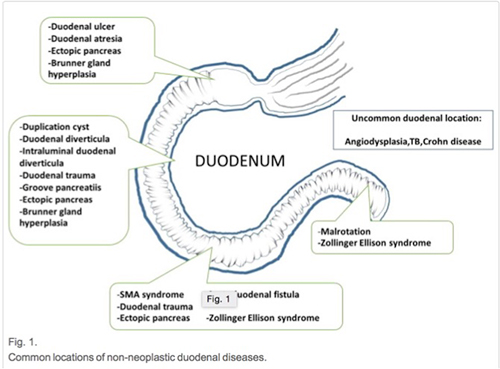
- “Ectopic pancreas, also known as heterotopic pancreatic tissue, is defined as aberrant pancreatic tissue with no ductal or vascular continuity to the main pancreatic gland. Most patients are asymptomatic and this disorder is typically found incidentally. Ectopic pancreas is normally located in the submucosal layer of the stomach, duodenum, and/or jejunum and may easily be misconstrued as a submucosal tumor, such as a gastrointestinal stromal tumor (GIST).”
Imaging Spectrum of Non-neoplastic Duodenal Diseases Sitthipong S et al. Clinical Imaging (in press)
- “The duodenum can be involved in several major polyposis syndromes, including familial adenomatous polyposis (FAP), Peutz Jeghers syndrome, Cronkite Canada syndrome, and juvenile polyposis. Duodenal polyps are commonly found in patients with Cronkite Canada syndrome, which shows similarities to juvenile polyposis, but polyps are usually small and more diffuse. Ectodermal changes, such as alopecia and nail dystrophy; and inflammatory infiltrate in lamina propria are associated with Cronkite Canada syndrome. Polyps associated with Cronkite Canada syndrome are more commonly sessile than pedunculated.”
Imaging Spectrum of Non-neoplastic Duodenal Diseases Sitthipong S et al. Clinical Imaging (in press)
- “Duodenal trauma is rare, accounting for less than 2% of all abdominal trauma. Penetrating injury is the most common mechanism of duodenal injury, followed by blunt injury in the form of duodenal compression against the vertebral columns. CT is the imaging method of choice for assessment of duodenal trauma for many reasons, including nonspecific clinical presentation, frequently absence of peritoneal signs due to retroperitoneal location, and detection of associated injuries. Associated injuries include pancreatic, hepatic, renal, and splenic injuries, which are more common than isolated duodenal injury. Intramural hematoma, contusion, and perforation are the important spectral duodenal trauma.”
Imaging Spectrum of Non-neoplastic Duodenal Diseases Sitthipong S et al. Clinical Imaging (in press)
- “Superior mesenteric artery syndrome (SMA syndrome) is an uncommon pathology that is caused by compression of the third part of the duodenum between the SMA and aorta. It is also known as Wilkie syndrome. Clinical manifestations related to proximal duodenal obstruction include epigastric pain, weight loss, nausea, and vomiting. Pain relief may be achieved by lying in the prone or left lateral decubitus position . Predisposing factors include rapid weight loss that causes loss of retroperitoneal fat, scoliosis, and body cast – all of which alter the angle between SMA and aorta.”
Imaging Spectrum of Non-neoplastic Duodenal Diseases Sitthipong S et al. Clinical Imaging (in press) - “Aortoduodenal fistula can be classified as being either primary or secondary. Primary ADF is defined as direct communication between distal duodenum and native aorta. The fixed retroperitoneal third portion of the duodenum makes it the most common location for fistula formation with aorta. The most common cause of primary ADF is atherosclerotic aortic aneurysm. Less common causes of primary ADF include tuberculosis, mycotic infection, Takayasu disease, and collagen vascular disease. Periaortic inflammatory process and adhesion between duodenum and aorta may be possible mechanisms for fistula formation.”
Imaging Spectrum of Non-neoplastic Duodenal Diseases Sitthipong S et al. Clinical Imaging (in press) - “Vasculitis that involves the gastrointestinal tract is usually part of a systemic disease, such as systemic lupus erythematosus (SLE), polyarteritis nodosa (PAN), and Wegener's granulomatosis. Clinical course depends on the size and location of the affected vessel. Manifestations of vasculitis with large vessel involvement may be indistinguishable from those of mesenteric ischemia. With medium-size vessel involvement, segmental inflammation and erosion may lead to aneurysmal formation, which commonly occurs in PAN. Gastrointestinal hemorrhage caused by aneurysmal rupture is the associated complication.”
Imaging Spectrum of Non-neoplastic Duodenal Diseases Sitthipong S et al. Clinical Imaging (in press)
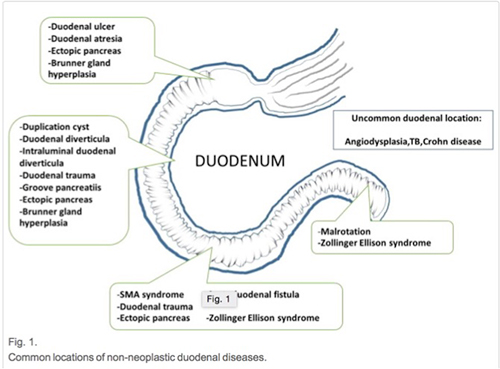
- “ Duodenal atresia, the most common congenital gastrointestinal obstruction, is caused by a failure of recanalization of the intestinal tract during the second month of fetal life. Infants with duodenal atresia present with bilious vomiting early in the neonatal period. The atretic segment is most often just beyond the ampulla of Vater. If the atresia is proximal to the ampulla of Vater, the vomiting is nonbilious. Atresia is complete in 40% to 60% of cases. It is commonly associated with prematurity (46%), maternal polyhydramnios (33%), Down syndrome (24%), annular pancreas (33%) and malrotation (28%).”
Imaging Spectrum of Non-neoplastic Duodenal Diseases Sitthipong S et al. Clinical Imaging (in press) - “Normal position of duodenojejunal flexure is to the left of the left-sided pedicles of the vertebral body at the level of the duodenal bulb on frontal views. The advantage of CT is to show not only intestinal malrotation (i.e., duodenojejunal flexure fails to cross the midline and locates below the level of the duodenal bulb), but also to detect other associated extra-intestinal imaging features, such as reverse location of superior mesenteric artery (SMA) and vein. This is a useful indicator; however, some patients will have normal vascular orientation.”
Imaging Spectrum of Non-neoplastic Duodenal Diseases Sitthipong S et al. Clinical Imaging (in press) - “Important complications are mid-gut volvulus and ischemic change from torsion of small bowel on shortened mesentery. However, normal anatomic variations that mimic malrotation may be encountered on frontal views, in particular on the upper GI series. Common variations include laxity of ligament of Treitz due to ageing process; displacement by splenomegaly, liver transplantation, and renal agenesis; and, inferior displacement of duodenojejunal flexure in premature infant due to relatively mobile ligament of Treitz by the adjacent distended stomach or bowel. False-negative findings due to misinterpretation of the duodenal course as indication of normal variation rather than malrotation have been reported.”
Imaging Spectrum of Non-neoplastic Duodenal Diseases Sitthipong S et al. Clinical Imaging (in press) - “Paraduodenal hernia is the most common type of internal hernia that can be classified as a congenital type and normal aperture subtype. It is characterized by a protrusion of small bowel into the retroperitoneal space through defects in the peritoneum near the third and fourth part of the duodenum. There are two types - right and left, with the latter observed in about 75% of cases. Both types manifest with nonspecific symptoms, such as postprandrial pain, vomiting, and bowel obstruction. Left paraduodenal hernia occurs when bowel protrudes through Landzert's fossa, which is located posterior to the fourth part of the duodenum.”
Imaging Spectrum of Non-neoplastic Duodenal Diseases Sitthipong S et al. Clinical Imaging (in press) - “Duodenal duplication cyst most frequently occurs at the medial wall of the second and third part of the duodenum. It typically appears as a well-circumscribed cystic lesion with fluid density that does not communicate with the duodenal lumen. Microscopically, it is a cyst that is lined with mucosa and that is surrounded by a muscular layer. Duodenal duplication cyst is a congenital malformation resulting from incomplete recanalization of the alimentary tract during early fetal life. Its discovery is mostly incidental; however, it may occasionally cause biliary obstruction, pancreatitis, or superimposed infection. In rare cases, carcinoma can occur within the duplication cysts.”
Imaging Spectrum of Non-neoplastic Duodenal Diseases Sitthipong S et al. Clinical Imaging (in press) - “The duodenum is the second most common site of diverticula after the colon, formed by pulsion of the mucosa and submucosa that herniate through the muscular defect. Duodenal diverticula often occur at the medial wall of the second part of duodenum, and they rarely become inflamed in contrast to diverticula occurring elsewhere in the bowel, due to their larger size and the regular flow of relatively sterile and liquid luminal contents. However, diverticulitis, perforation, or hemorrhage may be encountered. Biliary tract complication or so-called Lemmel syndrome, which is defined as obstructive jaundice caused by juxtapapillary or periampullary diverticulum, can occur if located within 2.5 cm of the ampulla of Vater.”
Imaging Spectrum of Non-neoplastic Duodenal Diseases Sitthipong S et al. Clinical Imaging (in press) - “By way of an important clinical consideration, difficulty may be encountered in cannulation of the bile duct during endoscopic retrograde cholangiopancreatography (ERCP) if the ampulla drains into the diverticulum. This condition is easy to diagnose if the diverticulum is full of air, but may be confused and misinterpreted as pancreatic cystic tumor or choledochal cyst if the lumen is completely filled with fluid. Continuity between duodenal lumen and diverticula is a helpful imaging feature.”
Imaging Spectrum of Non-neoplastic Duodenal Diseases Sitthipong S et al. Clinical Imaging (in press) - “Intraluminal duodenal diverticula (IDD) usually occur in the second or third part of the duodenum. IDD are formed by aberration of embryologic luminal recanalization and are comprised of diaphragm or web within the lumen of duodenum. An aperture allows movement of some food contents through the diaphragm, but duodenal peristalsis and intraluminal pressure lead to progressive ballooning of the diaphragm. The classic appearance on barium examination is windsock sign. The usefulness of CT to diagnose IDD has recently been reported. CT combined with post-processing software, such as curve planar reformation, can nicely depict the IDD and their attachment.”
Imaging Spectrum of Non-neoplastic Duodenal Diseases Sitthipong S et al. Clinical Imaging (in press) - “Duodenitis is defined as inflammation of duodenal mucosa with no discrete ulcer formation. This condition has both infectious and noninfectious causes. The most common infectious cause is Helicobacter pylori. Other potential infectious causes include mycobacterium tuberculosis and cryptosporidium. Cryptosporidium Duodenitis is exclusively seen in HIV patients. Two main noninfectious causes are alcohol and NSAIDs abuse.”
Imaging Spectrum of Non-neoplastic Duodenal Diseases Sitthipong S et al. Clinical Imaging (in press) - “Duodenal ulcer is normally caused by Helicobacter pylori infection, it occurs most frequently in the duodenal bulb, and it is more common than gastric ulcer. Classic features on barium examination include solitary or multiple pockets of barium filling the ulcer crater , edematous collar of mucosal swelling (in contrast to rolled edges of malignant ulcer), and radiating folds of mucosa at the edge of the ulcer. Complications include stricture, bleeding, and perforation. CT is the modality of choice in cases of perforated duodenal ulcer. Duodenal wall thickening, periduodenal fluid, and retroperitoneal air or free intraperitoneal air are the important imaging findings on CT in perforated duodenal ulcer.”
Imaging Spectrum of Non-neoplastic Duodenal Diseases Sitthipong S et al. Clinical Imaging (in press)
Stomach
- “Heterotopic pancreas represents a congenital anomaly where aberrant pancreatic tissue is without ductal or vascular continuity to the gland. The reported incidence ranges from 0.55–13.7%,however, the true incidence is unknown as most patients are asymptomatic and the condition is usually an incidental finding at autopsy or laparotomy. Most ectopic pancreatic tissue is found incidentally during evaluation of other organs. Common sites of involvement include the upper portions of the gastrointestinal tract including the stomach, duodenum, and proximal jejunum.”
Heterotopic pancreas: typical and atypical imaging findings J.W. Kung et al. Clinical Radiology 65 (2010) 403–407 - “However, most individuals remain asymptomatic clinically and are detected during surgery or endoscopy for another evaluation. When symptoms do occur the majority are related to a combination of mass effect and the local and systemic complications of activated pancreatic enzymes.15 Other possible presentations include obstruction from duodenal or pyloric stricture, gastrointestinal hemorrhage, or elevation in serum amylase and lipase..”
Heterotopic pancreas: typical and atypical imaging findings J.W. Kung et al. Clinical Radiology 65 (2010) 403–407 - “Heterotopic pancreas is most often incidentally discovered in the upper gastrointestinal tract, with the stomach
being the most common location. Lesions in the stomach range from 1–3 cm and are usually located along the greater
curvature in the gastric antrum within 6cm of the pylorus.”
Heterotopic pancreas: typical and atypical imaging findings J.W. Kung et al. Clinical Radiology 65 (2010) 403–407 - “At CT a prospective diagnosis of heterotopic pancreas is challenging. Masses are often oval or round with smooth or serrated margins in the gastric antral wall. Often there is homogeneous early enhancement, similar to the normal pancreas. Occasionally, poor enhancement is seen, in which case lesions have been shown to consist primarily of ducts and hypertrophied muscle. A minority of cases show dilatation of heterotopic pancreatic duct.”
Heterotopic pancreas: typical and atypical imaging findings J.W. Kung et al. Clinical Radiology 65 (2010) 403–407
- “Gastric pneumatosis , also referred to as gastric emphysema or emphysematous gastritis, is the least common site of pneumatosis within the gastrointestinal tract, seen in 9% of cases in a single review of 86 patients with gastrointestinal pneumatosis on CT. The term gastric pneumatosis encompasses both gastric emphysema and emphysematous gastritis, with the latter referring specifically to the uncommon, though life-threatening, infectious variant. Dependent tiny locules or linear collections of gas within the dependent gastric wall raise concern for pneumatosis, though gas within the rugae may mimic true pneumatosis. Correlation with sagittal and coronal reconstructions as well as persistence between arterial and portal venous phases may aid in diagnosis.”
Nonmalignant gastric causes of acute abdominal pain on MDCT: a pictorial review. Fung CI, Fishman EK Abdom Radiol (NY). 2016 Aug 1. [Epub ahead of print] - “While gastritis may diffusely involve the stomach, focal, and segmental thickening can alternatively be seen, particularly in the setting of Helicobacter pylori infection or with medications such as nonsteroidal anti-inflammatory drugs (NSAIDs). NSAID-induced gastritis occurs secondary to decreased prostaglandin synthesis, resulting in decreased mucus and bicarbonate secretion with subsequent gastric injury. Focal gastritis or ulcers secondary to NSAIDs or other medications classically occur along the gastric body and antrum along the greater curvature due to their dependent position. Focal wall thickening may mimic neoplasm; due to the overlap between MDCT appearance and gastric neoplasm, endoscopy is often required for definitive diagnosis.”
Nonmalignant gastric causes of acute abdominal pain on MDCT: a pictorial review. Fung CI, Fishman EK Abdom Radiol (NY). 2016 Aug 1. [Epub ahead of print] - “A number of causes of gastric pneumatosis have been described including infection, ischemia, medications, endoscopic procedures, and idiopathic. MDCT may aid in determining the underlying cause and directing
52-year-old man, acute abdominal pain. Axial venous phase MDCT. Perforating ulcer (long arrow) arising from the stomach antrum (S) with gastric content filling the lesser sac and secondary pneumoperitoneum (short arrow).
subsequent management. Early endoscopy with gastric biopsy can similarly help determine the underlying etiology, particularly in differentiating infectious and non- infectious causes. Elevated lactate has been associated with increased mortality on one multivariate analysis.”
Nonmalignant gastric causes of acute abdominal pain on MDCT: a pictorial review. Fung CI, Fishman EK Abdom Radiol (NY). 2016 Aug 1. [Epub ahead of print] - “Gastric ulcers are common and often result from H. pylori infection or medications, especially NSAIDs. Superficial ulcers are not typically well visualized on MDCT; however, deep or penetrative ulcers may be appreciated. Secondary inflammation can result in adjacent wall thickening or other soft tissue change. Extraluminal gas or pneumoperitoneum may be present in cases of perforation.”
Nonmalignant gastric causes of acute abdominal pain on MDCT: a pictorial review. Fung CI, Fishman EK Abdom Radiol (NY). 2016 Aug 1. [Epub ahead of print] - “Upper gastrointestinal bleeding accounts for approximately 0.1% of hospitalizations in the USA each year, with a mortality rate of 10%. Common causes of gastric hemorrhage include ulcers, varices, Mallory– Weiss tears, vascular lesions, and neoplasms. Clinical presentation varies depending on the degree of blood loss, ranging from asymptomatic with less than 00 mL/day to systemic shock if greater than 15% of the circulating blood volume is lost. Contrast-enhanced MDCT may allow direct visualization of the bleeding site via high-attenuating contrast extravasation. In the absence of contrast, high-attenuating debris within the stomach fundus can suggest ongoing or prior hemorrhage, particularly in hospitalized patients without recent ingestion with unexplained anemia or abdominal pain.”
Nonmalignant gastric causes of acute abdominal pain on MDCT: a pictorial review. Fung CI, Fishman EK Abdom Radiol (NY). 2016 Aug 1. [Epub ahead of print] - “Although uncommon, foreign body ingestion may result in dramatic imaging findings. Foreign body ingestions are most common in children, the intellectually disabled, and individuals with predisposing factors or injurious situational problems (e.g., suicidal ideation, anxiety, alcohol abuse, etc.). Clinical history is critical and MDCT is often performed to exclude complications. The vast majority of objects pass through the gastrointestinal tract without issue. Elongate or sharp objects have increased risk of perforation or obstruction. Secondary complications including mediastinitis, peritonitis, abscess formation, or sepsis may occur following perforation. High-risk objects including sharp or large foreign bodies may require endoscopic or surgical removal.”
Nonmalignant gastric causes of acute abdominal pain on MDCT: a pictorial review. Fung CI, Fishman EK Abdom Radiol (NY). 2016 Aug 1. [Epub ahead of print] - “Unlike the majority of gastrointestinal fistulae, which are often iatrogenic or related to inflammatory bowel disease, gastrocolic fistulae are most commonly caused by penetrating benign ulcers in the setting of NSAID use. Neoplasm and inflammation are less common causes. Classically patients present with acute halitosis, feculent vomiting, and undigested food, though the most common clinical presentation is nonspecific abdominal pain.”
Nonmalignant gastric causes of acute abdominal pain on MDCT: a pictorial review. Fung CI, Fishman EK Abdom Radiol (NY). 2016 Aug 1. [Epub ahead of print] - “Most commonly seen in elderly women with a history of biliary disease, gallstone-associated gastric outlet obstruction—or ‘‘Bouveret’s Syndrome’’—is a rare condition caused by retrograde passage of a large gallstone into the duodenum or stomach with subsequent obstruction. Although the least common location for gallstones to become lodged, early recognition or duodenal or gastric gallstone obstruction is critical due to a reported mortality of 30%. MDCT or radiographs may aid in the diagnosis prior to invasive assessment through visualization of the gallstone or secondary features including pneumobilia and gastric distension; however, endoscopy is diagnostic. As with the related condition of gallstone ileus, management is surgical.”
Nonmalignant gastric causes of acute abdominal pain on MDCT: a pictorial review. Fung CI, Fishman EK Abdom Radiol (NY). 2016 Aug 1. [Epub ahead of print]
Vascular
- OBJECTIVE. The objective of the present study is to quantify the diagnostic yield of triple-rule-out (TRO) CT for the evaluation of acute chest pain in emergency department patients.
CONCLUSION. In 8.9% of patients, TRO CT detected a significant noncoronary diagnosis that could explain acute chest pain, including pathologic findings that would not be identified on dedicated coronary CT angiography.
Diagnostic Yield of Triple-Rule-Out CT in an Emergency Setting Amelia M. Wnorowski, Ethan J. Halpern AJR 2016; 207:295–301 - “Acute coronary syndrome (ACS) accounts for a minority of acute chest pain presentations and was diagnosed in only 13% of patients who visited the emergency department for chest pain in 2007–2008 . However, ACS is a serious cause of chest pain, with an associated mortality rate of 3–33% and high associated morbidity, because up to 30% of patients with ACS who are discharged from the emergency department are rehospitalized within 6 months.”
Diagnostic Yield of Triple-Rule-Out CT in an Emergency Setting Wnorowski AM, Halpern EJ AJR 2016; 207:295–301 - “For the diagnosis of coronary artery disease, TRO CT has a sensitivity of 94.3%, a specificity of 97.4%, and a negative predictive value of 99%, findings that are similar to those obtained with the use of dedicated coronary CTA .”
Diagnostic Yield of Triple-Rule-Out CT in an Emergency Setting Wnorowski AM, Halpern EJ AJR 2016; 207:295–301 - “Although coronary disease was the most common diagnosis that explained chest pain, accounting for chest pain in 11.7% of our emergency department patients, TRO CT identified noncoronary diagnoses that could explain the presentation in 8.9% of our patient population. Pulmonary embolism was the most commonly noted noncoronary diagnosis.”
Diagnostic Yield of Triple-Rule-Out CT in an Emergency Setting Wnorowski AM, Halpern EJ AJR 2016; 207:295–301 - “On the basis of our retrospective review of CT findings, 30 (27.3%) of the patients with significant noncoronary diagnoses (28 of whom had pulmonary embolism and two of whom had an aortic pathologic finding) would not have been identified with the use of dedi- cated coronary CTA because of unopacified right-side circulation or limited z-axis cover- age (in patients with aortic pathologic find- ings).”
Diagnostic Yield of Triple-Rule-Out CT in an Emergency Setting Wnorowski AM, Halpern EJ AJR 2016; 207:295–301 - “In our patient population, more than 80% of patients had negative study results without significant coronary or noncoronary diagnoses. This is similar to the results of a previous study, in which 76% of patients did not require further testing. In the same study, TRO CT had a negative predictive value of 99.4% and was associated with no adverse outcomes.”
Diagnostic Yield of Triple-Rule-Out CT in an Emergency Setting Wnorowski AM, Halpern EJ AJR 2016; 207:295–301 - “Our experience with close to 1200 consecutive TRO CT studies over 10 years found that TRO CT identified significant and potentially fatal noncoronary diagnoses in 8.9% of the presenting population. The frequency of these noncoronary diagnoses is dependent on an appropriately selected patient population with a low to intermediate risk of ACS and for whom alternative diagnoses should also be considered, including pulmonary embolism and acute aortic pathology. TRO CT also identifies patients at risk for ACS and allows discharge of a majority of patients with negative study results.”
Diagnostic Yield of Triple-Rule-Out CT in an Emergency Setting Wnorowski AM, Halpern EJ AJR 2016; 207:295–301