Imaging Pearls ❯ April 2016
|
-- OR -- |
|
Chest
- “Septic pulmonary embolism is an uncommon disease in which septic thrombi are mobilised from an infectious nidus and transported in the vascular system of the lungs. It is usually associated with tricuspid valve vegetation, septic thrombophlebitis or infected venous catheters.”
Septic pulmonary embolism associated with a peri-proctal abscess in an immunocompetent host Chang E et al. BMJ Case Rep. 2009; 2009: bcr07.2008.0592. - “Septic pulmonary embolism is an uncommon disease in which thrombi containing microorganisms in a fibrin matrix are mobilised from an infectious nidus and transported in the venous system to implant in the vascular system of the lungs. It is usually associated with tricuspid valve vegetation, septic thrombophlebitis or infected venous catheters. Less common infection with the potential for septic pulmonary embolism is postanginal septicaemia, sometimes referred to as Lemierre’s syndrome,and periodontal disease..”
Septic pulmonary embolism associated with a peri-proctal abscess in an immunocompetent host Chang E et al. BMJ Case Rep. 2009; 2009: bcr07.2008.0592. - “Septic pulmonary emboli reach the lung from a variety of sources, including infected heart valves, peripheral sites of septic thrombophlebitis, and infected venous cathetersor pacemaker wires. In the intravenous drug user, the most common cause of septic emboli is tricuspid valve endocarditis.”
Pulmonary septic emboli: diagnosis with CT. Kuhlman JE, Fishman EK, Teigen C Radiology. 1990 Jan;174(1):211-3. - “The CT scans of 18 patients with documented pulmonary septic emboli were reviewed. CT features of septic emboli included multiple peripheral nodules ranging in size from 0.5 to 3.5 cm (15 of 18 patients [83%]), a feeding vessel sign (n = 12; [67%]), cavitation (n = 9; [50%]), wedge-shaped peripheral lesions abutting the pleura (n = 9 [50%]), air bronchograms within nodules (n = 5 [28%]), and extension into the pleural space (n = 7 [39%]). In six of the 18 patients, CT was the first modality (before radiography) to show lesions compatible with septic emboli.”
Pulmonary septic emboli: diagnosis with CT. Kuhlman JE, Fishman EK, Teigen C Radiology. 1990 Jan;174(1):211-3.
Colon
- “The term pseudomyxoma peritonei is a clinical or radiologic description rather than a pathologic diagnosis. Pseudomyxoma peritonei (or jelly belly) describes the finding of copious, thick mucinous or gelatinous material on the surfaces of the peritoneal cavity.”
Secondary Tumors and Tumorlike Lesions of the Peritoneal Cavity: Imaging Features with Pathologic Correlation Levy AD et al. RadioGraphics 2009; 29:347–373 - “Pseudomyxoma peritonei is a rare condition with a reported incidence of one case per mil- lion population per year. It occurs more commonly in women than men.The mean age of patients at diagnosis is 49 years (range, 23–83 years). Patients typically complain of pro- gressive abdominal pain, increasing abdominal girth, and weight loss. In some cases, patients complain of predominantly right-sided pain or they may have signs and symptoms similar to those of appendicitis when pseudomyxoma peritonei is located predominantly in the right lower quadrant.”
Secondary Tumors and Tumorlike Lesions of the Peritoneal Cavity: Imaging Features with Pathologic Correlation Levy AD et al. RadioGraphics 2009; 29:347–373 - “Scalloping of the visceral surfaces of the intra- peritoneal organs is an important diagnostic finding that helps differentiate pseudomyxoma from simple ascites. Scalloping represents the indentations that occur on the capsular margins of the intraperitoneal organs from the extrinsic pressure of the intraperitoneal mucinous implants. It is most commonly observed along the margins of the liver and spleen.”
Secondary Tumors and Tumorlike Lesions of the Peritoneal Cavity: Imaging Features with Pathologic Correlation Levy AD et al. RadioGraphics 2009; 29:347–373
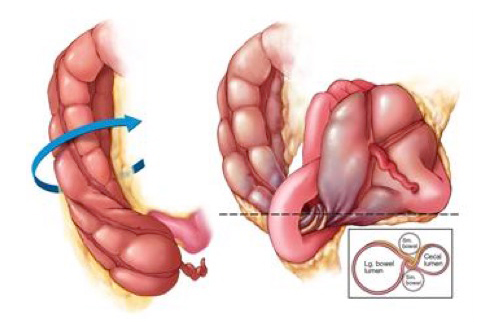
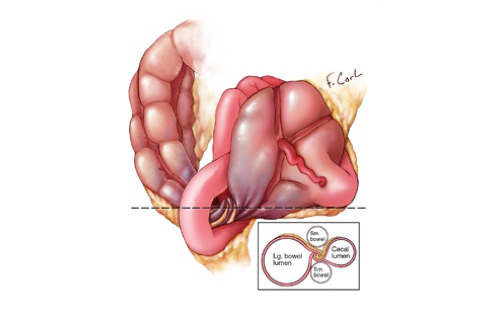
- Cecal Volvulus
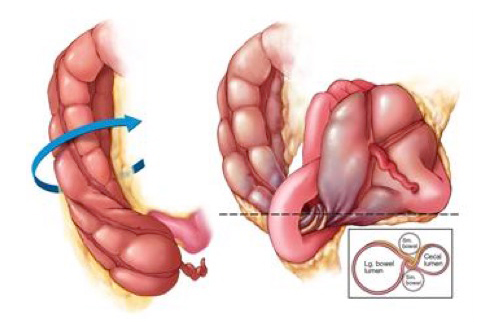
- Cecal Volvulus
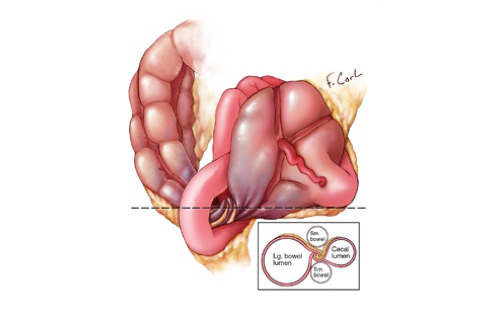
- “Volvulus of the cecum is a torsion of the bowel around its own mesentery that often results in a closed- loop obstruction. Cecal volvulus can only occur in the small percentage (11–25%) of the population who have a developmental failure of peritoneal fixation, allowing the proximal colon to be free and mobile. The second requirement is restriction of the bowel at a fixed point within the abdomen that serves as a fulcrum for rotation, such as an adhesion, abdominal mass, or scarring
from calcified lymph nodes.“
CT of Cecal Volvulus: Unraveling the Image Carolyn J. Moore, Frank M. Corl, Elliot K. Fishman AJR Am J Roentgenol. 2001 Jul;177(1):95-8 - “Cecal volvulus accounts for 11% of all in- testinal volvulus, generally occurring in pa- tients who are 30–60 years old. Medical history of these patients may include prior abdominal surgery, presence of a pelvic mass, violent coughing, atonia of the colon, extreme exertion, unpressurized air travel, or third-trimester pregnancy. Patients present with nausea, vomiting, constipation, and acute cramping pain.” CT of Cecal Volvulus: Unraveling the Image Carolyn J. Moore, Frank M. Corl, Elliot K. Fishman AJR Am J Roentgenol. 2001 Jul;177(1):95-8
- “Three-dimensional imaging is ideal because, like a barium enema, the entire bowel can be visualized in a single image, separating the volvulus from other dilated loops. Three-dimensional displays allow radiologists to select the optimal plane for viewing the volvulus and to locate the precise
source of the torsion . In effect, the ability to analyze an image in multiple planes allows one to unravel twisted bowel and confirm the diagnosis of volvulus. .”
CT of Cecal Volvulus: Unraveling the Image Carolyn J. Moore, Frank M. Corl, Elliot K. Fishman AJR Am J Roentgenol. 2001 Jul;177(1):95-8 - “On axial CT images, cecal volvulus is sug- gested by the extreme dilatation of the cecum. When seen on conventional radiographs or to- mograms, the cecal volvulus is seen as a rounded focal collection of air-distended bowel with haustral creases in the left upper quadrant that resembles a coffee bean . The two limbs of the looped obstruction gradually taper and converge at the site of the torsion, resulting in the appearance of a bird’s bea.”
CT of Cecal Volvulus: Unraveling the Image Carolyn J. Moore, Frank M. Corl, Elliot K. Fishman AJR Am J Roentgenol. 2001 Jul;177(1):95-8 - “The reduction rates in cecal volvulus achieved through use of colonoscopy are much lower than those achieved in sigmoid volvulus, and in patients with cecal volvulus, the recurrence rate exceeds 50%. In patients with uncomplicated cecal volvulus, surgical options include cecopexy, which has a low rate of morbidity (0–8%) and volvulus recurrence.”
CT of Cecal Volvulus: Unraveling the Image Carolyn J. Moore, Frank M. Corl, Elliot K. Fishman AJR Am J Roentgenol. 2001 Jul;177(1):95-8
GU Misc
- “Germ cell tumours in men usually arise from the testes, with only 1–2% originating from other locations.These so-called primary extra-gonadal germ cell tumours (EGCTs) are rare, accounting for 0.15–0.2% of all malignancies.They are characterized by their midline location, and have been reported to occur anywhere from the pineal gland to the coccyx, with the commonest locations being the mediastinum and the retroperitoneum.”
Primary retroperitoneal seminoma: an unusual cause of testicular pain Malde S JRSM Open December 2010 vol. 1 no. 7 63 - “Retroperitoneal masses can be caused by a range of benign and malignant conditions. Commonly, these include metastatic lymphadenopathy, lymphoma and liposarcoma. However, retroperitoneal germ cell tumours are rare lesions, accounting for only 4.4% of all malignant primary retroperitoneal tumours.Half of these are seminomatous in nature.”
Primary retroperitoneal seminoma: an unusual cause of testicular pain Malde S JRSM Open December 2010 vol. 1 no. 7 63 - “Retroperitoneal seminomas are rare tumours, and it is difficult to know whether they are true primary tumours or metastases from an occult or regressed testicular primary. In many cases, patients may present with a variety of symptoms and imaging findings are often non-specific. Consequently, the diagnosis is commonly overlooked initially. We recommend that male patients with persistent non-specific genitourinary symptoms and normal testicular investigations undergo a CT scan to exclude the possibility of a retroperitoneal mass. Furthermore, if no testicular abnormality is found in patients confirmed to have an EGCT, regular testicular self-examination is advised to identify the development of tumour recurrence early..”
Primary retroperitoneal seminoma: an unusual cause of testicular pain Malde S JRSM Open December 2010 vol. 1 no. 7 63
Kidney
- “Angiomyolipoma is the most common benign solid renal neoplasm observed in clinical practice. Once thought to be a hamartoma and almost always diagnosed by the imaged-based detection of fat, angiomyolipomas are now known to consist of a heterogeneous group of neoplasms. Although all are considered perivascular epithelioid cell tumors, many display different pathology, imaging features, and clinical behavior. The importance of understanding this group of neoplasms is emphasized by the fact that many types of angiomyolipoma contain little to no fat, and despite being benign, sometimes escape a pre-operative diagnosis.”
Renal angiomyolipoma: a radiological classification and update on recent developments in diagnosis and management Jinzaki M et al. Abdom Imaging. 2014; 39(3): 588–604. - “Angiomyolipoma is a solid tumor that is encountered commonly in the kidney in clinical practice. Angiomyolipoma is typically a solid “triphasic” tumor composed of varying amounts of three elements: dysmorphic blood vessels, smooth muscle components, and mature adipose tissue . Because most angiomyolipomas contain substantial amounts of adipose tissue, it is usually diagnosed using CT or MRI by identifying imaging features of fat cells in the mass.”
Renal angiomyolipoma: a radiological classification and update on recent developments in diagnosis and management Jinzaki M et al. Abdom Imaging. 2014; 39(3): 588–604. - “The term perivascular epithelioid cell tumors (PEComa) was introduced by Zamboni et al. in 1996. In 2002 and 2003, two monographs published under the auspices of the WHO recognized a family of neoplasms with perivascular epithelioid cell (PEC) differentiation and coined the term, “PEComa” . PEComas are mesenchymal neoplasms composed of nests and sheets of predominantly epithelioid and some spindle cells that are associated with blood vessel walls, and the perivascular epithelioid cell or “PEC” (a cell that has no known normal tissue counterpart).”
Renal angiomyolipoma: a radiological classification and update on recent developments in diagnosis and management Jinzaki M et al. Abdom Imaging. 2014; 39(3): 588–604. - “Triphasic angiomyolipoma is a benign mesenchmal tumor composed of varying amounts of dysmorphic blood vessels, smooth muscle components, and mature adipose tissue. It occurs sporadically in less than 0.2% of people , typically during the 4th to 6th decade of life, and exhibits a female preponderance. Triphasic angiomyolipoma can be divided radiologically into “classic” and “fat poor subtypes.”
Renal angiomyolipoma: a radiological classification and update on recent developments in diagnosis and management Jinzaki M et al. Abdom Imaging. 2014; 39(3): 588–604. - “The image-based detection of fat often begins with CT . On unenhanced CT, the presence of regions of interest (ROI)-containing attenuations less than −10 HU allows the confident identification of fat . The CT appearance of a classic angiomyolipoma varies due to variable amounts of fat, blood vessels, and smooth muscle components of the neoplasm. These neoplasms do not contain smooth muscle; they reveal smooth muscle-like cells (hence the term “components”) which typically stain positive for HMB-45 and smooth muscle markers. When evaluating angiomyolipomas with a small amount of fat with CT, the acquisition of thin (1.5–3 mm) sections and obtaining attenuation measurements using small ROI or even pixel values may be necessary to detect fat that otherwise would not be detected because of partial volume-averaging.”
Renal angiomyolipoma: a radiological classification and update on recent developments in diagnosis and management Jinzaki M et al. Abdom Imaging. 2014; 39(3): 588–604. - “A fat-containing mass that originates in the kidney is likely an angiomyolipoma rather than liposarcoma. Identification of enlarged or bridging vessels, aneurysms, and perinephric hematomas are additional imaging features of angiomyolipoma that are rarely seen with liposarcoma.”
Renal angiomyolipoma: a radiological classification and update on recent developments in diagnosis and management Jinzaki M et al. Abdom Imaging. 2014; 39(3): 588–604. - “Some triphasic angiomyolipomas contain too little fat (i.e., too few fat cells) to be detected with unenhanced CT; some have been diagnosed pre-operatively as RCC and inadvertently removed at surgery. These subtypes are now collectively referred to as “fat poor angiomyolipomas”. By definition, these lesions do not reveal fat at unenhanced CT, even when thin (1.5–3 mm) sections are used. In 1997, the term “angiomyolipoma with minimal fat” was introduced to describe angiomyolipomas that were hyperattenuating relative to renal parenchyma on unenhanced CT, homogeneously enhancing, and at pathology were composed almost entirely of a smooth muscle component and little to no fat.”
Renal angiomyolipoma: a radiological classification and update on recent developments in diagnosis and management Jinzaki M et al. Abdom Imaging. 2014; 39(3): 588–604. - “Hyperattenuating angiomyolipoma is now the preferred term to describe a lesion that was originally described as an “angiomyolipoma with minimal fat”; these lesions represent approximately 4–5% of all angiomyolipomas . They are typically small and average 3 cm in diameter . At pathology, they generally contain only 4% (range, 3–10%) fat cells. The abundant smooth muscle component generally stains positive for HMB-45 antigen and smooth muscle markers.”
Renal angiomyolipoma: a radiological classification and update on recent developments in diagnosis and management Jinzaki M et al. Abdom Imaging. 2014; 39(3): 588–604. - “Because of the abundant smooth muscle component, all hyperattenuating angiomyolipomas are hyperattenuating relative to renal parenchyma on unenhanced CT (usually more than 45 HU) similar to smooth muscle elsewhere, and typically homogeneously enhancing on CT.”
Renal angiomyolipoma: a radiological classification and update on recent developments in diagnosis and management Jinzaki M et al. Abdom Imaging. 2014; 39(3): 588–604. - “Angiomyolipomas are observed in 55%–75% of patients with TSC; most form by the third decade . Relative to sporadic angiomyolipoma, both genders are affected equally. Angiomyolipomas in TSC typically present at a younger age, are more often multiple, larger, and almost always bilateral .”
Renal angiomyolipoma: a radiological classification and update on recent developments in diagnosis and management Jinzaki M et al. Abdom Imaging. 2014; 39(3): 588–604. - “Renal angiomyolipomas may also occur in patients with lymphangioleiomyomatosis (LAM), a rare disease characterized by proliferation of atypical smooth muscle-like cells with associated cystic changes. LAM typically presents with symptoms related to the destructive cystic changes in the lungs. The pulmonary disease is progressive and may result in pneumothoraces, chylous pleural effusions, and respiratory failure. LAM occurs sporadically or in association with TSC.”
Renal angiomyolipoma: a radiological classification and update on recent developments in diagnosis and management Jinzaki M et al. Abdom Imaging. 2014; 39(3): 588–604. - Renal Tumors that Contain Fat
• Angiomyolipoma
• Renal cell carcinoma
• Wilms tumor
• Teratoma
- “Late or delayed complications of renal trauma develop more than 4 weeks after injury and include hypertension, hydronephrosis, calculus formation, and chronic pyelonephritis.”
Kidney in Danger: CT Findings of Blunt and Penetrating Renal Trauma Alonso RC et al. RadioGraphics 2009; 29:2033–2053 - “Posttraumatic renovascular hypertension may occur anywhere from a few weeks to decades fol- lowing injury, but on average occurs within 34 months. Several mechanisms have been proposed for its development, including renal artery occlusion, stenosis (Goldblatt kidney),
or compression; severe renal contusion; arterio-venous fistula or pseudoaneurysm formation; and chronic contained subcapsular hematoma.”
Kidney in Danger: CT Findings of Blunt and Penetrating Renal Trauma Alonso RC et al. RadioGraphics 2009; 29:2033–2053 - “The term Page kidney refers to hypertension secondary to constrictive ischemic nephropathy caused by large chronic subcapsular hematomas, which exert a mass effect on the adjacent renal parenchyma, indenting or flattening the renal margin.This condition may lead to diminished renal perfusion, fibrosis, and scarring.”
Kidney in Danger: CT Findings of Blunt and Penetrating Renal Trauma Alonso RC et al. RadioGraphics 2009; 29:2033–2053 - “At CT, typical findings include a delayed nephrogram
of the kidney and a surrounding fibrotic band that may be calcified. Because spontaneous resolution of posttraumatic hypertension
has been reported in many studies, conservative and pharmacologic treatment is strongly advised. Surgery, including renal revascularization, partial nephrectomy, or even total nephrectomy, is the second step in the management of posttraumatic hypertension.”
Kidney in Danger: CT Findings of Blunt and Penetrating Renal Trauma Alonso RC et al. RadioGraphics 2009; 29:2033–2053 - “Approximately 10% of all significant blunt ab- dominal traumatic injuries manifest with renal injury, although it is usually minor. Contrast- enhanced CT is the imaging modality of choice in the evaluation and management of renal trauma, since it provides essential anatomic and func- tional information. Renal imaging is indicated in cases of (a) penetrating trauma and hematuria; (b) blunt trauma, shock, and hematuria; and
(c) gross hematuria.”
Kidney in Danger: CT Findings of Blunt and Penetrating Renal Trauma Alonso RC et al. RadioGraphics 2009; 29:2033–2053
Pancreas
- Vascular Pancreatic Tumors
• Neuroendocrine tumor
• Serous cystadenoma
• Metastases to the pancreas (RCC)
• SPEN tumor
- “Cystic fibrosis (CF) is the most common inher- ited fatal disease in whites, affecting approximately 1 in every 3500 children born yearly . Inheritance is autosomal recessive, and the gene mutations have been identified at a single locus on the long arm of chromosome 7. The CF gene and its product, the CF transmembrane conductance regulator (CFTR), cause abnormal chloride ion transport on the apical surface of exocrine gland epithelial cells. This results in abnormally thickened, viscous secretions, which affect multiple organ systems. Mucous plugging, bronchiectasis, and recurrent infection are the well-known pulmonary manifestations, with respiratory failure the most common cause of mortality.”
Review of the Abdominal Manifestations of Cystic Fibrosis in the Adult Patient Michael B. Robertson et al. RadioGraphics2006;26:679–690 - “Exocrine gland insufficiency affects 85%–90%
of all CF patients and is a result of inspissated secretions leading to proximal duct obstruction with subsequent acinar disruption and replacement by fibrous tissue and fat . Patients with CF diagnosed in adulthood are far more likely to be pancreatic enzyme sufficient than those with CF diagnosed in childhood. Those patients with residual pancreatic exo- crine function are prone to recurrent episodes of acute pancreatitis . Endocrine gland dysfunction is reported in 30%– 50% and is thought to result from fibrosis and gland atrophy.”
Review of the Abdominal Manifestations of Cystic Fibrosis in the Adult Patient Michael B. Robertson et al. RadioGraphics2006;26:679–690 - “Complete fatty replacement is the most common pancreatic finding at imaging in adult CF patients, and the mean age of fatty replacement is 17 years.”
Review of the Abdominal Manifestations of Cystic Fibrosis in the Adult Patient Michael B. Robertson et al. RadioGraphics2006;26:679–690 - “Pancreatic cysts are relatively common in CF patients, are usually small, measuring 1–3 mm, and are best demonstrated with T2- weighted MR imaging or MR cholangiopancreatography. Occasionally, aggregates of true epithelium-lined cysts completely replace the pancreas, a condition referred to as pancreatic cystosis. It is thought to occur when the functional secretory capacity of the gland is maintained in the presence of ductal obstruction.”
Review of the Abdominal Manifestations of Cystic Fibrosis in the Adult Patient Michael B. Robertson et al. RadioGraphics2006;26:679–690 - “ Pancreatic carcinoma, although uncommon in CF patients, is one of the digestive tract malignancies for which CF patients are at increased risk.”
Review of the Abdominal Manifestations of Cystic Fibrosis in the Adult Patient Michael B. Robertson et al. RadioGraphics2006;26:679–690
Practice Management
- “Social media is defined as a ‘set of interactive technology tools designed to encourage social networking and dialogic communication in virtual communities and networks’. Social media platforms include online forums, networking sites, online professional networks, content posting sites and research forums . A recently published comprehensive analysis of social media encourages health care staff to embrace the ‘e-society’ and social media revolution as it has shown to provide improved outcomes for healthcare staff and patients.”
Social media in clinical radiology: have you updated your status? Kassamali RH, Palkhi EYA, Hoey ET Quant Imaging Med Surg. 2015 Aug; 5(4): 491–493. - “The revolution in social media enables radiologists to showcase their roles and responsibilities in the healthcare setting, and provides an interface to engage with patients and other healthcare members. Social media can therefore be a tool to improve patient education; this can be in the form of twitter feeds or health blogs tailored to discuss essential or topical issues in the media or local community .”
Social media in clinical radiology: have you updated your status? Kassamali RH, Palkhi EYA, Hoey ET Quant Imaging Med Surg. 2015 Aug; 5(4): 491–493. - “From a patient perspective, the increased self-education through social media risks the possibility of becoming unnecessarily or inadequately concerned, due to lack of sufficient knowledge or contradicting information on social media; this can jeopardize patient safety especially if some patients use the social media as a replacement for traditional forms of consultation.”
Social media in clinical radiology: have you updated your status? Kassamali RH, Palkhi EYA, Hoey ET Quant Imaging Med Surg. 2015 Aug; 5(4): 491–493. - “The results show that 85 % of all survey participants are using social media, mostly for a mixture of private and professional reasons. Facebook is the most popular platform for general purposes, whereas LinkedIn and Twitter are more popular for professional usage. The most important reason for not using social media is an unwillingness to mix private and professional matters. Eighty-two percent of all participants are aware of the educational opportunities offered by social media.”
Radiologists' Usage of Social Media: Results of the RANSOM Survey. Ranschaert ER et al. J Digit Imaging. 2016 Feb 3. [Epub ahead of print] - “An increasing number of hospitals and health systems utilize social media to allow users to provide feedback and ratings. The correlation between ratings on social media and more conventional hospital quality metrics remains largely unclear, raising concern that healthcare consumers may make decisions on inaccurate or inappropriate information regarding quality.”
Hospital Evaluations by Social Media: A Comparative Analysis of Facebook Ratings among Performance Outliers. Glover M et al. J Gen Intern Med. 2015 Oct;30(10):1440-6 - “Hospitals performing better than the national average on 30-day readmissions were more likely to use Facebook than lower-performing hospitals (93.3 % vs. 83.5 %; p < 0.01). The average rating for hospitals with low readmission rates (4.15 ± 0.31) was higher than that for hospitals with higher readmission rates (4.05 ± 0.41, p < 0.01). Major teaching hospitals were 14.3 times more likely to be in the high readmission rate group. A one-star increase in Facebook rating was associated with increased odds of the hospital belonging to the low readmission rate group by a factor of 5.0 (CI: 2.6-10.3, p < 0.01), when controlling for hospital characteristics and Facebook-related variables.”
Hospital Evaluations by Social Media: A Comparative Analysis of Facebook Ratings among Performance Outliers. Glover M et al. J Gen Intern Med. 2015 Oct;30(10):1440-6 - “The most important reason for not using social media is an unwillingness to mix private and professional matters. Eighty-two percent of all participants are aware of the educational opportunities offered by social media. The survey results underline the need to increase radiologists' skills in using social media efficiently and safely. There is also a need to create clear guidelines regarding the online and social media presence of radiologists to maximize the potential benefits of engaging with social media.”
Radiologists' Usage of Social Media: Results of the RANSOM Survey. Ranschaert ER et al. J Digit Imaging. 2016 Feb 3. [Epub ahead of print] - “Hospitals with lower rates of 30-day hospital-wide unplanned readmissions have higher ratings on Facebook than hospitals with higher readmission rates. These findings add strength to the concept that aggregate measures of patient satisfaction on social media correlate with more traditionally accepted measures of hospital quality.”
Radiologists' Usage of Social Media: Results of the RANSOM Survey. Ranschaert ER et al. J Digit Imaging. 2016 Feb 3. [Epub ahead of print]
Small Bowel
- “Ganglioneuroma is a rare tumor which should nevertheless be included in differential diagnosis of retroperitoneal masses when presenting as a well-delimited tumor with possible tendency to surround or displace major blood vessels, low density on non-enhanced CT, and delayed progressive enhancement on CT and MRI.”
Imaging of retroperitoneal ganglioneuroma Otal P et al. May 2001, Volume 11, Issue 6, pp 940-945 - “Various types of neurogenic tumors can affect the abdomen. These tumors can be classified as being of ganglion cell origin (ganglioneuromas, ganglioneuroblastomas, neuroblastomas), paraganglionic system origin (pheochromocytomas, paragangliomas), or nerve sheath origin (neurilemmomas, neurofibromas, neurofibromatosis, malignant nerve sheath tumors).”
Neurogenic Tumors in the Abdomen: Tumor Types and Imaging Characteristics Sung Eun Rha et al. RadioGraphics2003;23:29–43 - “Ganglioneuromas are rare, benign neurogenic tumors that arise from sympathetic ganglia. The tumors are composed of mature Schwann cells, ganglion cells, and nerve fibers. Ganglioneuromas may arise anywhere along the paravertebral sympathetic plexus and occasionally from the adrenal medulla. The retroperitoneum (32%–52% of cases) and posterior mediastinum (39%– 43%) are the two most common locations for a ganglioneuroma, followed by the cervical region (8%– 9%).”
Neurogenic Tumors in the Abdomen: Tumor Types and Imaging Characteristics Sung Eun Rha et al. RadioGraphics2003;23:29–43 - “Ganglioneuromas are often asymptomatic even if they are large. Otherwise, abdominal pain or the palpation of an abdominal mass is the most common clinical feature. Hormonally active forms have been reported, and the secretion of catecholamines, vasoactive intestinal polypeptides, or androgenic hormones explains such symptoms as hypertension, diarrhea, and virilization.”
Neurogenic Tumors in the Abdomen: Tumor Types and Imaging Characteristics Sung Eun Rha et al. RadioGraphics2003;23:29–43 - “At unenhanced CT, the tumors appear homogeneous, with an attenuation less than that of muscle. At CT, they contain calcification in about 20% of cases. The calcifications are discrete and punctate rather than amorphous and coarse as in neuroblastomas . Varying degrees of contrast material enhancement in
ganglioneuroma have been reported, from slight to moderate to marked.”
Neurogenic Tumors in the Abdomen: Tumor Types and Imaging Characteristics Sung Eun Rha et al. RadioGraphics2003;23:29–43 - “Ichikawa et al reported an interesting contrast enhancement pattern in ganglioneuroma that consisted of delayed heterogeneous uptake . These enhancement features are explained by the presence of an abundance of myxoid matrices in the tumors, resulting in delayed progressive accumulation of contrast material in the extracellular space.”
Neurogenic Tumors in the Abdomen: Tumor Types and Imaging Characteristics Sung Eun Rha et al. RadioGraphics2003;23:29–43
- “Tumors of small intestine account for only 1%-2% of all gastrointestinal tumors, and benign tumors account for approximately 30% of all small intestinal tumors. Gastrointestinal stromal tumors are the most common symptomatic benign tumors of the small bowel, while the lipomas are rare benign tumors, representing 2.6% of non-malignant tumors of the intestinal tract.”
Small intestinal lipomas: Diagnostic value of multi-slice CT enterography Song-Hua Fang et al. World J Gastroenterol. 2010 Jun 7; 16(21): 2677–2681. - “Small bowel lipomas tend to occur in the elderly, and the sixth to seventh decades of life are considered to be the most risky period. Jejunum and ileum, especially the terminal ileum, are common locations. Eleven of the 15 lesions arose from jejunoileum and the mean age of the patients was 63.2 years in this study, which was consistent with those previously reported. Patients may be completely asymptomatic with small lipomas (< 1 cm), which are usually detected incidentally. Larger tumors may produce symptoms .”
Small intestinal lipomas: Diagnostic value of multi-slice CT enterography Song-Hua Fang et al. World J Gastroenterol. 2010 Jun 7; 16(21): 2677–2681. - “Approximately 25% of patients with benign intestinal neoplasm have alimentary tract hemorrhage. Small bowel lipomas usually cause lower gastrointestinal hemorrhage, and lipomas arising from duodenum may cause upper gastrointestinal hemorrhage and symptoms like peptic ulcer. Some of the bleeding is intermittent, some is continuous in small amount or only presents as microscopically positive fecal occult blood.”
Small intestinal lipomas: Diagnostic value of multi-slice CT enterography Song-Hua Fang et al. World J Gastroenterol. 2010 Jun 7; 16(21): 2677–2681. - “Abdominal CT scans are considered to be the most definitive diagnostic measure of recognizing small bowel lipomas. With the fast volume scan technique of multiple spiral CT, reformation in any dimensions is feasible, and the quality of the reformatted images is almost as same as the axial ones, which ensures a good overall observation. The finding of lipid attenuation (-100 to -50 HU) is vital to the diagnosis of a lipoma.”
Small intestinal lipomas: Diagnostic value of multi-slice CT enterography Song-Hua Fang et al. World J Gastroenterol. 2010 Jun 7; 16(21): 2677–2681.
- Small Bowel Intussuception: Causes in Adults
• Transient and intermittent (idiopathic)
• Small bowel tumors
• Ingested foreign bodies
• Enteric tubes
• Meckel’s diverticulum - “Adult intussusception is thought to be rare, accounting for an estimated 5% of all intussusceptions and only 1% of small-bowel obstructions. Unlike intussusceptions in children, which are idiopathic in 90% of cases, adult intussusceptions were tradition- ally thought to have an identifiable cause in the majority of cases.”
MDCT and 3D Imaging in Transient Enteroenteric Intussusception: Clinical Observations and Review of the Literature Horton KM, Fishman EK AJR 2008; 191:736–742 - “Intussusception occurs when a segment (intussusceptum) of the gastrointestinal tract invaginates (or telescopes) with its mesenter- ic fold into the adjacent segment (intussus- cipiens). This telescoping results from altered peristalsis, which pulls the intussusceptum into the intussuscipiens. A variety of factors can act as a lead point and result in intussus- ception, including tumors, ingested foreign bodies, enteric tubes or suture material, and Meckel’s diverticulum.”
MDCT and 3D Imaging in Transient Enteroenteric Intussusception: Clinical Observations and Review of the Literature Horton KM, Fishman EK AJR 2008; 191:736–742 - “Intussusception can occur anywhere along the gastrointestinal tract. Gastric intussusception is very rare. Enteroenteric intussusceptions are much more common than gastric intussusception and result when one loop of small bowel invaginates into the adjacent small bowel. They can be categorized as du- odenojejunal, jejunojejunal, or jejunoileal. Large-bowel intussusception can be classified as ileocolic or colocolic and has a high report- ed association with underlying tumors.”
MDCT and 3D Imaging in Transient Enteroenteric Intussusception: Clinical Observations and Review of the Literature Horton KM, Fishman EK AJR 2008; 191:736–742 - “Ileocecal intussusceptions, which are typically classified as a colonic intussusception, are reported to be the most common of all the gastrointestinal intussusceptions, although enteroenteric intussusceptions can account for up to 40% of cases.”
MDCT and 3D Imaging in Transient Enteroenteric Intussusception: Clinical Observations and Review of the Literature Horton KM, Fishman EK AJR 2008; 191:736–742 - “Malignant lesions include carcinoid, metastases, leiomyosarcoma, and adenocarcinoma. Benign tumors that have been re- ported to result in intussusception include lipoma, neurofibroma, hemangioma, and inflammatory polyps. Meckel’s diverticulum is also a well-documented cause of small-bowel intussusception, often ileocecal.”
MDCT and 3D Imaging in Transient Enteroenteric Intussusception: Clinical Observations and Review of the Literature Horton KM, Fishman EK AJR 2008; 191:736–742 - “In asymptomatic patients, the CT identification of a proximal (jejunal), short (< 3.5 cm) intussusception with a char- acteristic target sign and without obstruction may indicate a self-limiting process that can be managed conservatively.”
MDCT and 3D Imaging in Transient Enteroenteric Intussusception: Clinical Observations and Review of the Literature Horton KM, Fishman EK AJR 2008; 191:736–742
Stomach
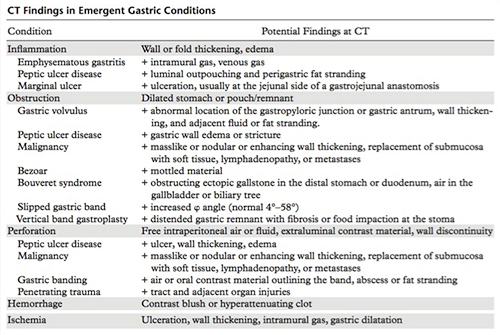
- “In an adequately distended stomach, the normal nondependent gastric body is less than or equal to 5 mm in thickness. The antral wall, in contrast, may normally measure less than or equal to 12 mm in thickness.”
CT of Gastric Emergencies Guniganti PG et al. RadioGraphics 2015; 35:1909–1921
- “In all cases of penetrating trauma, it is crucial to identify the injury tract. The stomach often collapses around the site of injury, so that a defect is not visible at imaging, making the injury tract the only sign of gastric trauma.”
CT of Gastric Emergencies Guniganti PG et al. RadioGraphics 2015; 35:1909–1921 - “Arterial supply to the stomach comes from all three branches of the celiac axis: the left gastric, common hepatic, and splenic arteries, forming two arterial arcades. Numerous anastomoses make the stomach relatively resistant to ischemia.”
CT of Gastric Emergencies Guniganti PG et al. RadioGraphics 2015; 35:1909–1921
- “Air in the gastric wall can be seen in a benign form of gastric emphysema, which can be encountered in the setting of a recent procedure and is typically asymptomatic. Patients with benign gastric emphysema demonstrate few clinical symptoms, whereas emphysematous gastritis causes patients to present with severe pain and potentially with sepsis and shock.”
CT of Gastric Emergencies Guniganti PG et al. RadioGraphics 2015; 35:1909–1921 - “The term gastric volvulus implies at least 180° rotation of the stomach and gastric outlet obstruction. Coronal reformatted images are particularly helpful in diagnosing gastric volvulus and often show these findings to greater advantage than axial images alone. Organoaxial or mesenteroaxial rotation of the stomach alone does not define volvulus.”
CT of Gastric Emergencies Guniganti PG et al. RadioGraphics 2015; 35:1909–1921 - “Gastritis is most frequently secondary to Helicobacter pylori infection, nonste- roidal anti-inflammatory drugs (NSAIDs), alcohol, or systemic illness. Patients with gastritis may present with epigastric pain, nausea, vomiting, or loss of appetite. Although CT, given its poor mucosal detail, is not the preferred modality for as- sessing gastritis, it is often the first study performed in patients with acute symptoms and may suggest the diagnosis.” CT of Gastric Emergencies Guniganti PG et al. RadioGraphics 2015; 35:1909–1921
- “Air in the gastric wall can be seen in a benign form of gastric emphysema, which can be encountered in the setting of a recent procedure and is typically asymptomatic. Patients with benign gastric emphysema demonstrate few clinical symptoms, whereas emphysematous gastritis causes patients
to present with severe pain and potentially with sepsis and shock. In addition to obtaining an appropriate history, absence of gastric wall edema is helpful in diagnosing benign gastric emphysema. The appearance of the intramural gas in benign gastric emphysema is often linear .”
CT of Gastric Emergencies Guniganti PG et al. RadioGraphics 2015; 35:1909–1921 - “Gastric volvulus is twisting of the stomach resulting in gastric outlet obstruction, and can result in ischemia or perforation. Patients classically present with sudden epigastric pain, intractable retching, and inability to pass a naso-gastric tube (the Borchardt triad).Volvulus occurs most often in elderly patients with a hiatal hernia and may be acute or chronic-recurrent. Paraesophageal hernias, particularly large type III hernias, are at greater risk of gastric volvulus.”
CT of Gastric Emergencies Guniganti PG et al. RadioGraphics 2015; 35:1909–1921 - “Gastric perforation can also occur with a gastric malignancy, particularly in ulcer- ated masses such as those seen with adenocar- cinoma, lymphoma, and large gastrointestinal stromal tumors (GISTs). Perforation from gastric adenocarcinoma typically occurs in patients more than 65 years of age with advanced stage disease. In patients with lower stage disease, a focal ulcerated mass can perforate if the ulceration is deep. Ulcerated gastric lymphoma can also result in gastric perforation, although small bowel perforation is more common.”
CT of Gastric Emergencies Guniganti PG et al. RadioGraphics 2015; 35:1909–1921 - “Gastric hemorrhage can be seen in a variety of gastric diseases, including PUD, tumor, varices, gastritis, and arteriovenous malformations. Patient presentation is variable, ranging from asymptomatic to hypovolemic shock. Direct signs of bleeding in- clude hematemesis, coffee-ground emesis, melena, or, in the setting of rapid bleeding, hematochezia. Although endoscopy is the preferred method of
diagnosing and treating upper gastrointestinal bleeding, CT is useful in cases where endoscopy is not clinically feasible or is nondiagnostic.”
CT of Gastric Emergencies Guniganti PG et al. RadioGraphics 2015; 35:1909–1921 - “CT findings of gastric hemorrhage include intraluminal contrast blush from active bleeding or hyperattenuating clot from recent bleeding. Clots in these cases are often seen in the fundus, which is the most dependent location in the supine patient. The location of the highest- attenuation clot (the sentinel clot) can indicate the source of bleeding. Hyperattenuating material in the stomach, including ingested material such as residual contrast medium or medications, surgical material, or foreign bodies, can potentially result in both false-positive and false-negative studies by mimicking or obscuring bleeding.”
CT of Gastric Emergencies Guniganti PG et al. RadioGraphics 2015; 35:1909–1921 - “Gastric ischemia is an uncommon condition caused by diffuse or focal vascular insufficiency. Although the extensive collateral blood supply to the stomach is protective, systemic hypotension (as is seen in sepsis or shock) may result in gastric ischemia. Other described causes of gastric ischemia include celiac and mesenteric stenosis, vasculitis, and disseminated thrombo- embolism. Imaging findings in gastric ischemia range from focal ulceration to gastric wall thickening to intramural gas. Ischemic ulcerations most commonly occur along
the anterior and posterior gastric walls near the anastomoses between the two arterial arches over the lesser and greater curvatures. Gastric dilatation may also be seen and is thought to be due to ischemic gastroparesis.”
CT of Gastric Emergencies Guniganti PG et al. RadioGraphics 2015; 35:1909–1921 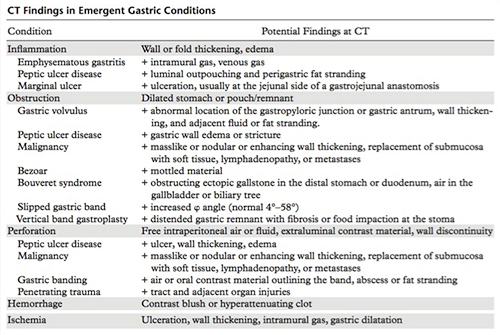
- “Varices cause approximately 30% of all episodes of upper gastrointestinal tract bleeding. CT angiography should be considered when endoscopy does not reveal a bleeding source and when there is a suspicion of arterial bleeding or a source in the lower gastrointestinal tract.”
Multidetector CT Angiography for Acute Gastrointestinal Bleeding: Technique and Findings José M. Artigas et al. RadioGraphics 2013; 33:1453–1470 - “Upper gastrointestinal tract bleeding may also occur in patients who are hospitalized for other causes; stress ulcers can appear within 24 hours of admission in a patient who has suffered severe trauma or burns.”
Multidetector CT Angiography for Acute Gastrointestinal Bleeding: Technique and Findings José M. Artigas et al. RadioGraphics 2013; 33:1453–1470 - “CT angiography is usually performed when endoscopy is not feasible or is nondiagnostic, but in most cases, CT angiography can be completed while preparing for endoscopy. Even when active hemorrhage has ceased, CT findings may assist in risk stratification and may be helpful in selecting the best option for definitive treatment, as well as its optimal timing.”
Multidetector CT Angiography for Acute Gastrointestinal Bleeding: Technique and Findings José M. Artigas et al. RadioGraphics 2013; 33:1453–1470 - “Acute GI bleeding can have arterial and venous sources. Venous bleeding within the upper GI tract is typically due to gastric or esophageal varices in the setting of portal hypertension. However, nearly 30% of patients with portal hypertension who have upper GI bleeding will have an arterial source of bleeding .The most common causes of upper GI bleeding are erosion or peptic ulcer disease. Multidetector CT angiography can also help diagnose rare bleeding related to interventional endoscopic procedures such as endoscopic sphincterotomy of the ampulla.”
Multidetector CT Angiography in Acute Gastrointestinal Bleeding: Why, When, and How Geffroy Y et al. RadioGraphics 2011; 31:35–E47 - “Acute gastrointestinal (GI) bleeding is a common major medical emergency with an annual incidence of 40–150 episodes per 100,000 persons for upper GI bleeding and 20–27 episodes per 100,000 persons for lower GI bleeding. In as many as 75% of cases, bleeding ceases spontaneously; however, bleeding can recur in 25% of cases, causing substantial morbidity and mortality.”
Multidetector CT Angiography in Acute Gastrointestinal Bleeding: Why, When, and How Geffroy Y et al. RadioGraphics 2011; 31:35–E47 - “Upper GI bleeding occurs proximal to the liga- ment of Treitz (which connects the fourth portion of the duodenum to the diaphragm) and arises from the esophagus, stomach, or duodenum. Lower GI bleeding involves the small bowel, colon, or rectum.”
Multidetector CT Angiography in Acute Gastrointestinal Bleeding: Why, When, and How Geffroy Y et al. RadioGraphics 2011; 31:35–E47 - “Inadequate gastric distention limits diagnostic evaluation of the stomach and poses a potential pitfall, as it may create a false appearance of thickening or, conversely, may obscure true disease. When evaluating abnormal gastric wall thickening in a nondistended stomach, supplementary findings can be helpful in identifying disease.”
CT of Gastric Emergencies Guniganti PG et al. RadioGraphics 2015; 35:1909–1921 - “The CT features of gastritis can overlap with malignancy. Certain features, such as the presence of mural stratification, favor inflammation, but when gastritis is focal or nodular in appearance, endoscopy and biopsy are often needed to exclude malignancy.”
CT of Gastric Emergencies Guniganti PG et al. RadioGraphics 2015; 35:1909–1921
- Benign gastric tumors
• Although these lesions demonstrate different histologic findings, the overlap of radiologic findings in many gastric tumors makes differentiation difficult.
• Clinical manifestations also overlap and can vary from severe abdominal pain and acute abdomen to vague signs such as weight loss and anemia.
• some gastric tumors cause diagnostic confusion, which may result in unnecessary surgery or inappropriate follow-up.
• some unusual gastric tumors have characteristic radiologic features that may suggest a specific diagnosis. - Lipoma
• Benign submucosal tumor composed of mature adipose tissue.
• 2%–3% of benign gastric tumors
• Usually detected incidentally.
• Large lipomas may have ulcerations as a result of pressure necrosis of the overlying mucosa and cause gastrointestinal bleeding.
• Can cause intussusception or bowel obstruction.
• Tend to occur as solitary lesions
• Most frequently in the gastric antrum - Gastric Duplications
• 7% of gastrointestinal tract duplications.
• Most are noncommunicating, spheric or ovoid closed cysts, and the most common site is the greater curvature
• The mucosal lining is usually gastric, but pseudostratified respiratory epithelium and pancreatic tissue have been found
• The clinical picture depends on their size and location as well as the presence of communication with the rest of the alimentary tract.
• Most duplications are discovered in infants. Vomiting and abdominal pain are the predominant clinical findings, although patients are frequently asymptomatic.
• US and CT show a well-defined cystic mass lying close to the greater curvature of the stomach. The presence of an echogenic inner rim and hypoechoic outer muscle layers is highly suggestive of a duplication - Leiomyoma
• Mesenchymal tumors of the gastrointestinal tract are usually incidentally discovered as a firm, protruding submucosal lesion during upper gastrointestinal examinations for unrelated conditions
• The larger tumors may occasionally cause bleeding
• Pathologically, most of these tumors are composed of spindle cells and display smooth muscle differentiation.
• Gastric mesenchymal tumors are classified immunohistochemically as leiomyomas or GISTs
• In particular, the leiomyomas are defined as being desmin positive and c-kit (CD117) negative tumors and the GISTs are defined as being c-kit positive tumors. - Schwannoma
• Neurogenic tumors of the stomach are rare
• Approximately 4% of all benign gastric tumors
• The majority of these tumors are schwannomas
• Included in the smaller group of gastrointestinal mesenchymal tumors, which contains relatively well-differentiated tumors that are identical to those arising from the somatic soft tissue
• Usually appear as discrete submucosal masses that are indistinguishable from other mesenchymal tumors
• As they outgrow their blood supply, these lesions may undergo central necrosis and ulceration.
• Schwannomas and gastrointestinal stromal tumors that show differentiation toward neural elements are histologically different tumors, although the relation between them is not clear - Glomus Tumor
• The most common benign vascular tumors of the stomach
• Typically originate from glomus bodies, which are specialized arteriovenous communications that regulate skin temperature.
• Usually occur in the gastric antrum
• Typically single tumors
• The majority of affected patients are asymptomatic
larger lesions are likely to be ulcerated and may cause upper gastrointestinal bleeding.
• At radiology, these tumors appear as smooth submucosal masses with or without ulceration
• Occasionally, may contain tiny flecks of calcification
• Enhance strongly on early-phase - Heterotopic pancreas
• The incidence in autopsies ranges 0.5%-13.7
• more common at the age of 30-50 years with a male predominance
• The usual location is in the stomach in 25%-38% of the cases, duodenum in 17%-36%, jejunum in 15%-21.7% and rare in the esophagus, gallbladder, common bile duct, spleen, mesentery, mediastinum and fallopian tubes.
• Gastric lesions are discovered in the antrum in 85%-95%, either on the posterior or anterior wall, being more common along the greater curvature.
• CT usually non specific may demonstrate the lesion which enhances similarly with the normal pancreatic tissue - “Gastric lipoma is a rare lesion, ac- counting for only 5% of gastrointestinal tract lipomas and fewer than 1% of all gastric tumors. Most gastric lipomas are small asymptomatic lesions that are detected as incidental findings at autopsy. The tumor is composed of well- differentiated adipose tissue surrounded by a fibrous capsule. Most gastric lipomas are found in the submucosa, and most are located in the pyloric antrum.”
Imaging Characteristics of Gastric Lipomas in 16 Adult and Pediatric Patients Thompson WM et al. AJR 2003;181:981–985 - “When the tumors are large (> 3–4 cm), the most common clinical presentation is upper gastrointestinal hemorrhage, either chronic or acute, caused by ulceration of the neoplasm. Abdominal pain and ob- structive symptoms are also common, especially if there is endoluminal growth that could cause intussusception.”
Imaging Characteristics of Gastric Lipomas in 16 Adult and Pediatric Patients Thompson WM et al. AJR 2003;181:981–985 - “Gastric lipomas larger than 3 cm are usually symptomatic. The most common findings pre-viously reported in the literature —obstruction and gastrointestinal bleeding—were found in our series. In our 16 patients, abdominal pain was the most common symptom (eight patients, 50%), with gastrointestinal bleeding present in six patients (38%). In two patients (13%) with no abdominal symptoms,
the gastric lipomas were discovered incidentally on imaging studies performed for reasons other than upper gastrointestinal symptoms, an occurrence that is not rare in patients with gastric lipomas.”
Imaging Characteristics of Gastric Lipomas in 16 Adult and Pediatric Patients Thompson WM et al. AJR 2003;181:981–985 - “In conclusion, our review of data for 16 patients with proven gastric lipomas revealed two significant findings. First, on upper gastrointestinal examinations, lipomas have the appearance of any submucosal tumor; they are indistinguishable from gastrointestinal stroma tumors or lymphoma. Second, CT findings are specific for the diagnosis of gastric lipoma. CT should be used to characterize large submucosal masses before endoscopic biopsy is performed.”
Imaging Characteristics of Gastric Lipomas in 16 Adult and Pediatric Patients Thompson WM et al. AJR 2003;181:981–985
Trauma
- “Late or delayed complications of renal trauma develop more than 4 weeks after injury and include hypertension, hydronephrosis, calculus formation, and chronic pyelonephritis.”
Kidney in Danger: CT Findings of Blunt and Penetrating Renal Trauma Alonso RC et al. RadioGraphics 2009; 29:2033–2053 - “Posttraumatic renovascular hypertension may occur anywhere from a few weeks to decades fol- lowing injury, but on average occurs within 34 months. Several mechanisms have been proposed for its development, including renal artery occlusion, stenosis (Goldblatt kidney),
or compression; severe renal contusion; arterio-venous fistula or pseudoaneurysm formation; and chronic contained subcapsular hematoma.”
Kidney in Danger: CT Findings of Blunt and Penetrating Renal Trauma Alonso RC et al. RadioGraphics 2009; 29:2033–2053 - “The term Page kidney refers to hypertension secondary to constrictive ischemic nephropathy caused by large chronic subcapsular hematomas, which exert a mass effect on the adjacent renal parenchyma, indenting or flattening the renal margin.This condition may lead to diminished renal perfusion, fibrosis, and scarring.”
Kidney in Danger: CT Findings of Blunt and Penetrating Renal Trauma Alonso RC et al. RadioGraphics 2009; 29:2033–2053 - “At CT, typical findings include a delayed nephrogram
of the kidney and a surrounding fibrotic band that may be calcified. Because spontaneous resolution of posttraumatic hypertension
has been reported in many studies, conservative and pharmacologic treatment is strongly advised. Surgery, including renal revascularization, partial nephrectomy, or even total nephrectomy, is the second step in the management of posttraumatic hypertension.”
Kidney in Danger: CT Findings of Blunt and Penetrating Renal Trauma Alonso RC et al. RadioGraphics 2009; 29:2033–2053 - “Approximately 10% of all significant blunt ab- dominal traumatic injuries manifest with renal injury, although it is usually minor. Contrast- enhanced CT is the imaging modality of choice in the evaluation and management of renal trauma, since it provides essential anatomic and func- tional information. Renal imaging is indicated in cases of (a) penetrating trauma and hematuria; (b) blunt trauma, shock, and hematuria; and
(c) gross hematuria.”
Kidney in Danger: CT Findings of Blunt and Penetrating Renal Trauma Alonso RC et al. RadioGraphics 2009; 29:2033–2053