Imaging Pearls ❯ Pancreas ❯ Surgical Complications
|
-- OR -- |
|
- “Accurate diagnosis of postoperative complications requires a solid understanding of pancreatic anatomy, surgical indications, normal postoperative appearance, and expected postsurgical changes. The practicing radiologist should be familiar with the most common perioperative complications, such as anastomotic leak, abscess, and hemorrhage, and be able to differentiate these entities from normal anticipated postoperative changes such as seroma, edema and fat stranding at the surgical site, and perivascular soft-tissue thickening. In addition to evaluation of the primary operative fossa, imaging plays a fundamental role in assessment of the adjacent organ systems secondarily affected after pancreatic surgery, such as vascular, biliary, and enteric complications.”
Imaging after Pancreatic Surgery: Expected Findings and Postoperative Complications
Ayman H. Gaballah et al.
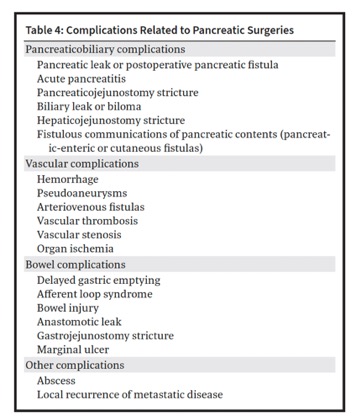
RadioGraphics 2024; 44(1):e230061 - • Complications often occur at the sites of surgical anastomoses, and knowledge of the surgical approach is critical for identifying the location and type of complication with imaging.
• Leakage of pancreatic juice can trigger the autodigestion of nearby structures, resulting in complications such as vascular erosion, hemorrhage, pseudoaneurysms, and fistulous communications with adjacent structures. Additionally, it is known to be associated with delayed gastric emptying, ileus, and infections, including abdominal abscesses and wound infections.
• Unexplained abdominal pain, features of pancreatic exocrine insufficiency, and attacks of acute pancreatitis in the late postoperative period associated with imaging findings of progressive pancreatic ductal dilatation and abrupt narrowing at the anastomotic site should raise concern for stricture formation
Imaging after Pancreatic Surgery: Expected Findings and Postoperative Complications
Ayman H. Gaballah et al.
RadioGraphics 2024; 44(1):e230061 - • Risk factors for anastomotic leak include preoperative radiation therapy, small size of the bile duct, and anastomosis of the CBD rather than the common hepatic duct to the jejunal loop. Pancreatic leak can also lead to bile leaks.
• Early-onset hemorrhage is due to surgical factors including inadequate hemostasis, slipped ligature, or fresh bleeding at a surgical site. It can occur due to arterial or venous injury or bleeding along the anastomotic siteor resected parenchymal surface. Late-onset hemorrhage can occur up to several days or weeks after surgery and generally has a pathologic cause.
Imaging after Pancreatic Surgery: Expected Findings and Postoperative Complications
Ayman H. Gaballah et al.
RadioGraphics 2024; 44(1):e230061 - “The pancreas mainly receives its blood supply from the celiac trunk and in part from the superior mesenteric artery (SMA). Typically the pancreatic head gets its arterial supply through the superior pancreaticoduodenal branches of the gastrodu-odenal artery and the inferior pancreaticoduodenal branches of the SMA. The body and tail receive their arterial supply predominantly from the dorsal pancreatic artery, which commonly arises from the splenic artery but may occasionally arise from the proximal proper hepatic artery or the celiac trunk. Additional small pancreatic branches from adjacent arteries, most of which arise from the splenic artery, also supply the body and tail.”
Imaging after Pancreatic Surgery: Expected Findings and Postoperative Complications
Ayman H. Gaballah et al.
RadioGraphics 2024; 44(1):e230061 - “The venous drainage of the pancreatic head passes through four pancreaticoduodenal veins. The posterior superior pancreaticoduodenal vein drains via the main portal vein. The anterior superior, anterior inferior, and posterior inferior pancreaticoduodenal veins drain via the SMV. The body and tail drain via tributaries predominantly into the splenic vein. Pancreatic lymphatic drainage mainly follows the arterial supply of the pancreas. The head drains into the pyloric nodes, and the body and tail drain into the pancreaticosplenic nodes. These lymph nodes drain into the celiac and superior mesenteric nodes.”
Imaging after Pancreatic Surgery: Expected Findings and Postoperative Complications
Ayman H. Gaballah et al.
RadioGraphics 2024; 44(1):e230061 - “CT is the primary imaging modality used for postoperative pancreatic imaging due to its excellent spatial resolution, short imaging time, and accurate depiction of air and calcifications. Additionally, CT angiography aids in detecting vascular complications. The CT protocol for postoperative surveillance should be multiphase. It should include contrast-enhanced imaging during the arterial phase (pancreatic parenchymal phase) at 40–50 seconds and portal venous phase at 65–70 seconds, which is also in line with the recommended protocol for preoperative evaluation.”
Imaging after Pancreatic Surgery: Expected Findings and Postoperative Complications
Ayman H. Gaballah et al.
RadioGraphics 2024; 44(1):e230061 - “Enlarged lymph nodes can manifest in the surgical bed in the postoperative period and can measure greater than 1 cm in diameter. These lymph nodes are rarely metastatic. They can be followed up at subsequent imaging to ensure stability or resolution.”
Imaging after Pancreatic Surgery: Expected Findings and Postoperative Complications
Ayman H. Gaballah et al.
RadioGraphics 2024; 44(1):e230061 - “It is widely regarded as the Achilles’ heel of pancreatic surgery owing to its potential to cause significant morbidity and mortality. Leakage of pancreatic juice can trigger the autodigestion of nearby structures, resulting in complications such as vascular erosion, hemorrhage, pseudoaneurysms, and fistulous communications with adjacent structures. Additionally, it is known to be associated with delayed gastric emptying, ileus, and infections, including abdominal abscesses and wound infections. In some cases, sepsis and multiorgan failure can also result from pancreatic leak.”
Imaging after Pancreatic Surgery: Expected Findings and Postoperative Complications
Ayman H. Gaballah et al.
RadioGraphics 2024; 44(1):e230061 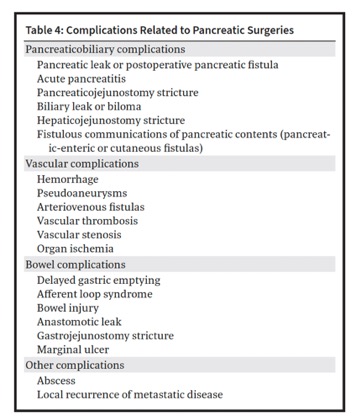
Imaging after Pancreatic Surgery: Expected Findings and Postoperative Complications
Ayman H. Gaballah et al.
RadioGraphics 2024; 44(1):e230061- “Pancreatic leak is the most common cause of pathologic fluid collection after surgery . The rate of clinically significant leak after distal pancreatectomy ranges from 5% to 40% in various studies. It is generally higher than the incidence observed after pancreaticoduodenectomy, which is reported to be between 6% and 14%. However, the leak following distal pancreatectomy tends to be less severe in terms of clinical impact than those following pancreaticoduodenectomy. The diagnosis of leak is essentially based on clinical and laboratory parameters and covers a spectrum ranging from a mild self-limiting leak to a severe or fatal leak.”
Imaging after Pancreatic Surgery: Expected Findings and Postoperative Complications
Ayman H. Gaballah et al.
RadioGraphics 2024; 44(1):e230061 - “Multiple vascular complications can occur after pancreatic surgery. These complications include hemorrhage, stenosis, thrombosis, graft occlusion, pseudoaneurysm formation, and organ ischemia and infarction. They are more common in patients undergoing vascular reconstructions, and risk increases with the complexity of the reconstruction Additionally, other postoperative complications and endovascular procedures can lead to the development of vascular complications.”
Imaging after Pancreatic Surgery: Expected Findings and Postoperative Complications
Ayman H. Gaballah et al.
RadioGraphics 2024; 44(1):e230061 - “The International Study Group of Pancreatic Surgery (ISGPS) developed a classification system for postpancreatic surgery hemorrhage. This system is based on three key parameters: the timing of onset (early vs late), the location of bleeding (intraluminal vs extraluminal), and the severity of the hemorrhage (mild vs severe). The ISGPS classification system further subdivides hemorrhage into three distinct grades. Specifically, grade A refers to mild early-onset hemorrhage within the first 24 hours after surgery, whereas grade B represents severe early-onset or any mild late-onset hemorrhage. Finally, grade C hemorrhage denotes severe late-onset hemorrhage.”
Imaging after Pancreatic Surgery: Expected Findings and Postoperative Complications
Ayman H. Gaballah et al.
RadioGraphics 2024; 44(1):e230061 - “Early-onset hemorrhage is due to surgical factors including inadequate hemostasis, slipped ligature, or fresh bleeding at a surgical site. It can occur due to arterial or venous injury or bleeding along the anastomotic site or resected parenchymal surface. Late-onset hemorrhage can occur up to several days or weeks after the surgery and generally has a pathologic cause. Anastomotic leaks (most commonly pancreatic leak) and postsurgical infection or abscess can lead to vascular erosions causing delayed hemorrhage. Arterial pseudoaneurysms and bleeding anastomotic ulcers can also cause delayed hemorrhage.”
Imaging after Pancreatic Surgery: Expected Findings and Postoperative Complications
Ayman H. Gaballah et al.
RadioGraphics 2024; 44(1):e230061 - “Active bleeding and pseudoaneurysms can be identified after intravenous contrast material injection and are ideally evaluated at CT angiography. With a sensitivity and specificity of 91% and 99%, respectively, arterial phase contrast-enhanced CT is highly effective in identifying the precise bleeding site. During the arterial phase, active extravasation may exhibit a jetlike or swirling appearance . Confirmation of the diagnosis can be achieved by observing contrast material pooling at the same site during the venous phase on dual-phase CT images .Patients whose condition is unstable may directly undergo conventional angiography for both diagnosis and therapy.”
Imaging after Pancreatic Surgery: Expected Findings and Postoperative Complications
Ayman H. Gaballah et al.
RadioGraphics 2024; 44(1):e230061 - “Bowel ischemia can also occur secondary to arterial or portal venous occlusion. In addition to the direct sign of vascular occlusion, other possible findings include bowel wall thickening, hemorrhage as evidenced by hyperattenuating bowel wall on unenhanced CT images, nonenhancement of the bowel wall, pneumatosis intestinalis, and portal venous gas. Ischemic gastropathy is a complication of an Appleby procedure and can manifest with refractory gastric ulcers, which may be complicated by bleeding or perforation. Beger and Frey procedures involve resection of the pancreatic head and may lead to ischemia of the CBD or duodenum owing to the possible disruption of their blood supply.”
Imaging after Pancreatic Surgery: Expected Findings and Postoperative Complications
Ayman H. Gaballah et al.
RadioGraphics 2024; 44(1):e230061 - “Seeding metastases, from pancreatic cancer following pancreatectomy or interventional procedures, is a rare complication with a few cases reported in the literature. In most cases, tumor recurrence occurred within the body wall at the laparotomy site, along the course of the postsurgical drain, or along the tract of a needle biopsy or percutaneous transhepatic biliary drainage catheter. Seeding metastasis within the posterior wall of the stomach has also been documented following an endoscopic US-guided fine needle aspiration of pancreatic cancer. The imaging features of the metastatic deposits can be similar to those of the primary tumor.”
Imaging after Pancreatic Surgery: Expected Findings and Postoperative Complications
Ayman H. Gaballah et al.
RadioGraphics 2024; 44(1):e230061
- Whipple Procedure
- Most common procedure for resection of tumor in the pancreatic head, uncinate process, and neck
- Also used for lesions of the ampulla, extrahepatic bile duct, duodenum and sometimes chronic pancreatitis
- Improvements in surgical technique and critical care
- Perioperative mortality rate now down to 1% at experienced centers, still significant morbidity - Whipple Procedure
- Classic Whipple
- Resection of the pancreatic head, neck, and uncinate process, duodenum, gallbladder, distal bile duct, and proximal jejunum
- Gastric antrum resected - Whipple Procedure
- Pylorus –Preserving Whipple
- Resection of the pancreatic head, neck, and uncinate process, duodenum, gallbladder, distal bile duct, and proximal jejunum
- Gastric antrum and 1st portion of duodenum are not resected - Post-Operative Hemorrhage
- Rare (4%), but well-known complication
- Mortality rate ranges up to 38%
- Can be intraluminal (within the bowel) (33%) or extraluminal (66%)
- initial presence of blood termed “sentinel” bleeding
- requires urgent evaluation, as bleeding implies the presence of a structural vascular abnormality or anastomotic dehiscence - Post-Operative Hemorrhage
- Two Types:
- “Early” post-operative hemorrhage
- First 24 hours after surgery
- Active bleeding at the gastroduodenal artery (GDA) stump as a result of inadequate ligation during surgery.
- “Late” post-operative hemorrhage
- Usually secondary to a vascular structural abnormality.
- Vascular erosions (hepatic artery, celiac artery, or splenic artery) and pseudoaneurysm formation
- Most common cause is abnormality of the GDA stump (either a pseudoaneurysm or active extravasation) .
- Very high association (up to 66%) with anastomotic breakdown - Post-Operative Hemorrhage
- “Early” post-operative hemorrhage
- First 24 hours after surgery
- Active bleeding at the gastroduodenal artery (GDA) stump as a result of inadequate ligation during surgery. - Post-Operative Hemorrhage
- “Late” post-operative hemorrhage
- Usually secondary to a vascular structural abnormality.
- Vascular erosions (hepatic artery, celiac artery, or splenic artery) and pseudoaneurysm formation
- Most common cause is abnormality of the GDA stump (either a pseudoaneurysm or active extravasation) .
- Very high association (up to 66%) with anastomotic breakdown
- Complications Post Whipples Procedure
- Pancreatic fistula
- Leaks From the Gastrojejunostomy
- Leaks From the Biliary-Enteric Anastomosis
- Abscesses
- Postoperative Hemorrhage
- Postoperative Pancreatitis
- Portal Vein and Superior Mesenteric Vein Thrombosis
- Hepatic Infarction
- Delayed Gastric Emptying
- Anastomotic Stricture
- Tumor Recurrence in the Surgical Bed - Complications Post Whipples Procedure
- Pancreatic fistula
- Leaks From the Gastrojejunostomy
- Leaks From the Biliary-Enteric Anastomosis
- Abscesses
- Postoperative Hemorrhage
- Postoperative Pancreatitis
- Portal Vein and Superior Mesenteric Vein Thrombosis
- Hepatic Infarction - “Pancreaticoduodenectomy, also referred to as the “Whipple” or “Kausch-Whipple” procedure, is the most common surgical procedure for the resection of tumors in the pancreatic head, uncinate process, and neck as well as lesions of the ampulla, extrahepatic bile duct, and duodenum. A procedure once associated with an extraordinarily high perioperative morbidity and mortality rate, improvements in surgical technique and critical care over the last three decades have reduced the perioperative mortality rate to as low as 1% in the highest-volume centers.”
CT after pancreaticoduodenectomy: spectrum of normal findings and complications.
Raman SP, Horton KM, Cameron JL Fishman EK.
AJR Am J Roentgenol. 2013 Jul;201(1):2-13. - What is a Whipple’s Procedure- (classic and pylorus preserving)
- Both of these surgeries involve resection of the pancreatic head, neck, and uncinate process as well as the duodenum, gallbladder, distal bile duct, and proximal jejunum. In almost all cases, a regional lymph node dissection is also performed.
- In the classic form of the Whipple procedure, the gastric antrum is removed, whereas the pylorus-preserving variant retains the gastric antrum and first portion of the duodenum. - CT Scan Protocol for Post Whipples Procedure
- Water is the usual oral contrast unless IV contrast can not be used
- IV contrast is mandatory to exclude any vascular related pathology
- Dual phase imaging is needed if a bleed is expected to define the site of bleed and determine its cause
- MPR and 3D imaging (especially MIP imaging) should be part of the routine interpretation protocol - Three anastomosis must be analyzed
- Pancreaticojejunostomy: A jejunal loop is most often anastomosed to the right of the pancreatic remnant, and the pancreatic duct can often be followed directly to the anastomosis.
- Hepaticojejunostomy or choledochojejunostomy: The biliary-enteric anastomosis can be difficult to appreciate in the axial plane, although pneumobilia can be a valu- able clue because gas in the intrahepatic bile ducts can be traced centrally toward the anastomosis and subsequently into the right upper quadrant bowel
- Gastrojejunostomy: At our institution, the jejunum is often anastomosed to the right of the gastric remnant, although the exact position of this anastomosis will undoubtedly vary depending on the institution and surgeon. - Pancreatic fistula (leak) is the single most important cause of morbidity and mortality after the Whipple procedure: The reported rate of pancreatic fistula may be anywhere between 6% and 14% (depending on the exact definition of a fistula that is used), and the mortality rate ranges from 1.4% to 3.7%.
- Pancreatic Fistula (leak)
- Pancreatic fistula (leak) is the single most important cause of morbidity and mortality after the Whipple procedure: The reported rate of pancreatic fistula may be anywhere between 6% and 14% (depending on the exact definition of a fistula that is used), and the mortality rate ranges from 1.4% to 3.7%. - Postoperative Hemorrhage
- Rare (4%) but has a high mortality rate (up to 38%)
- Early postoperative hemorrhage occurs within the first 24 hours after surgery and often results from active bleeding at the gastroduodenal artery (GDA) stump as a result of inadequate ligation during surgery
- Late postoperative hemorrhage occurs after 5 days and is usually secondary to a structural abnormality in the mesenteric vasculature. the most common cause of late bleeding remains an abnormality of the GDA stump (either a pseudoaneurysm or active extravasation).
- Late postoperative hemorrhage has a high association (perhaps up to 66%) with anastomotic breakdown (with associated vessel erosion) and sepsis. - Portal Vein and Superior Mesenteric Vein Thrombosis
- the diagnosis of portal vein-SMV thrombosis is not uncommonly overlooked on CT, particularly when the reader concentrates solely on the axial im- ages. The coronal images are often important for accurate diagnosis, particularly for thrombus in the SMV, and the SMV should be carefully evaluated in the coronal plane to search for short-segment filling defects that may be difficult to visualize on the axial source images. - “ The Whipple procedure is associated with a unique set of common complications, including pancreatic fistula, postsurgical hemorrhage, postoperative pancreatitis, portomesenteric venous thrombosis, hepatic infarction, delayed gastric emptying, and anastomotic strictures. Knowledge of these complications as well as a detailed understanding of normal postoperative anatomy and the normal CT appearance of the surgical bed and anastomoses is critical in arriving at the correct diagnosis.”
CT after pancreaticoduodenectomy: spectrum of normal findings and complications.
Raman SP, Horton KM, Cameron JL Fishman EK.
AJR Am J Roentgenol. 2013 Jul;201(1):2-13. - “ Knowledge of the cross-sectional anatomy following the Whipple procedure, and clinical findings for associated complications, are essential to rapidly and accurately diagnose such complications on postoperative studies in order to optimize treatment.”
Complications of Whipple surgery: imaging analysis
Bhosale P et al.
Abdom Imaging (2013) 38:273–284 - “Pancreaticoduodenectomy can be associated with severe morbidity requiring aggressive clinical management, and potentially surgical intervention. Complications such as POPF, biliary leak, and afferent loop obstruction can be identified by careful evaluation on cross-sectional imaging. Often, when complications are identified early, they can be managed successfully with less aggressive intervention than when recognized late.”
Complications of Whipple surgery: imaging analysis
Bhosale P et al.
Abdom Imaging (2013) 38:273–284 - “Early postoperative bleeding occurs within the first 24 h after surgery typically into the peritoneal or retroperitoneal regions usually from poorly secured and/or retracted vessels, or the reversal of vascular spasm in ‘‘unsealed’’ vessels, such as at the blind ending afferent loop or vessels which lie in close proximity to the portal vein or superior mesenteric artery.”
Complications of Whipple surgery: imaging analysis
Bhosale P et al.
Abdom Imaging (2013) 38:273–284
- “ Multidetector computed tomography is the modality of choice for identifying normal findings after surgery, postoperative complications, and tumor recurrence in patients who have undergone pancreatic surgery.”
Multidetector CT Evaluation of the Postoperative Pancreas
Yamauchi FI et al.
RadioGraphics 2012; 32:743-764 - Distal Pancreatectomy: Complications as Seen on CT
- Pancreatic fistulae
- Intraabdominal abscess
- Small bowel obstruction
- Post operative hemorrhage
- Splenic vein infarct extends to the portal vein
- Splenic infarct if splenectomy not performed
- Sites of Bleeding s/p Whipple’s Procedure: Therapy
- Embolism with coils, glue or absorbable gelatin sponge
- Coils
- Stent grafting
- Surgery - Sites of Bleeding s/p Whipple’s Procedure
- Gastroduodenal stump
- Common and proper hepatic artery erosions
- Celiac axis erosions
- Splenic artery erosions
- Inferior pancreatoduodenal artery aneurysm
- Arc of Buhler aneurysm and pseudoaneurysm (mesenteric collateral vessel that originates from common hepatic artery proximal to GDA) - Hemorrhagic Complications After Whipple Surgery: Facts
Early hemorrhage (with 24 hours) is due to GDA stump insufficiency due to technical failure
Late hemorrhage (after 24 hours) is caused by
- Ulcer
- Vascular erosion from pancreatic leak
- Fistula
- Pseudoaneurysm
- Anastomotic dehiscence - Whipple’s Procedure for Pancreatic Cancer: Early Complications
- Anastomotic leak
- Hemorrhage
- Sepsis
- Pancreaticojejunal fistulae
- Acute pancreatitis of the remnant pancreas
- peritonitis "Hemorrhagic complications occur in fewer than 10% of patients after Whipple pancreatoduodenectomy but account for as many as 38% of deaths. Bleeding typically occurs from the stump of the gastroduodenal artery, but other sites of bleeding are increasingly recognized."
Hemorrhagic Complications After Whipple Surgery: Imaging and Radiologic Intervention
Puppala S et al.
AJR 2011; 196:192-197