Imaging Pearls ❯ Colon ❯ Inflammatory Bowel Disease
|
-- OR -- |
|
- “The use of diverse types of drugs can result in a variety of acute and chronic complications that affect almost any organ. The bowel is one of the organs impacted by the side effects of medications. Imaging frequently plays a crucial role in the detection and characterization of complications occurring in the bowel. They include pseudomembranous colitis or antibiotic-associated colitis; angioedema induced by angiotensin-converting enzyme inhibitors; nonsteroidal anti-inflammatory drug-induced enteropathy; cocaine toxicity; clozapine-induced hypomobility; and bowel toxicity induced by chemotherapeutic agents. It is imperative that radiologists are fully aware of these complications and toxicities as well as the relevant findings.”
Drug‐induced bowel complications and toxicities: imaging findings and pearls
Sitthipong Srisajjakul et al.
Abdominal Radiology (2022) https://doi.org/10.1007/s00261-022-03452-1 - ”Pseudomembranous colitis (PMC) is a form of acute colitis. It usually presents as a complication of antibiotic treatment, especially clindamycin and second- and third-generation cephalosporins and fluoroquinolones. Other possible but less common causes of PMC are abdominal surgery, uremia, colonic obstruction, and prolonged hypotension. A clostridium difficile (C. difficile) infection with toxin production (toxins A [enterotoxin] and B [cytotoxin]) is the culprit in most cases of PMC. Pathologically, the toxins stimulate the immune system by recruiting neutrophils to invade the colonic mucosa.”
Drug‐induced bowel complications and toxicities: imaging findings and pearls
Sitthipong Srisajjakul et al.
Abdominal Radiology (2022) https://doi.org/10.1007/s00261-022-03452-1 - ”CT is immensely helpful in diagnosing PMC, particularly when the disease is not clinically suspected. The most common CT finding is wall thickening, which usually ranges from 3 to 32 mm in diameter (mean 14.7 mm). The degree of wall thickening is generally greater than other inflammatory or infectious forms of colitis, and is typically diffuse in distribution. The accordion sign, when detected, is highly suggestive of PMC, but it can only be detected in advanced cases.”
Drug‐induced bowel complications and toxicities: imaging findings and pearls
Sitthipong Srisajjakul et al.
Abdominal Radiology (2022) https://doi.org/10.1007/s00261-022-03452-1 - ”Imaging findings include diffuse thickening of the small bowel wall, hyperenhancement of the mucosal layer, and submucosal edema (target sign). Long segments of the small bowel tend to be involved, with a jejunal predilection. Other associated findings are fluid accumulation that results in dilatation of the small bowel lumen, preservation of luminal transit, mesenteric vascular engorgement, and ascites. Scheirey et al. described a straightened small bowel wall, which was believed to be related to a primary increase in tissue turgor (i.e., stiffening) of the small bowel wall.”
Drug‐induced bowel complications and toxicities: imaging findings and pearls
Sitthipong Srisajjakul et al.
Abdominal Radiology (2022) https://doi.org/10.1007/s00261-022-03452-1
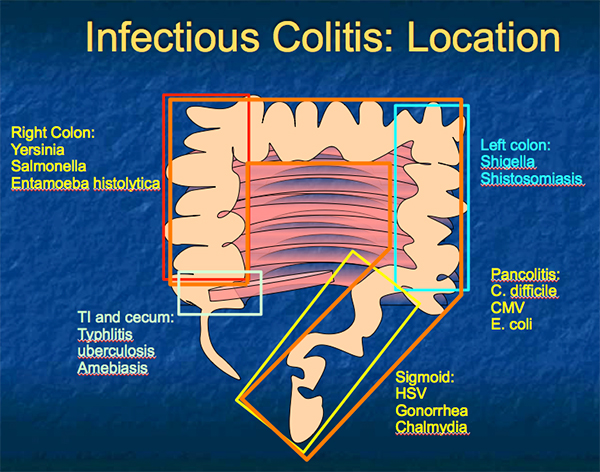
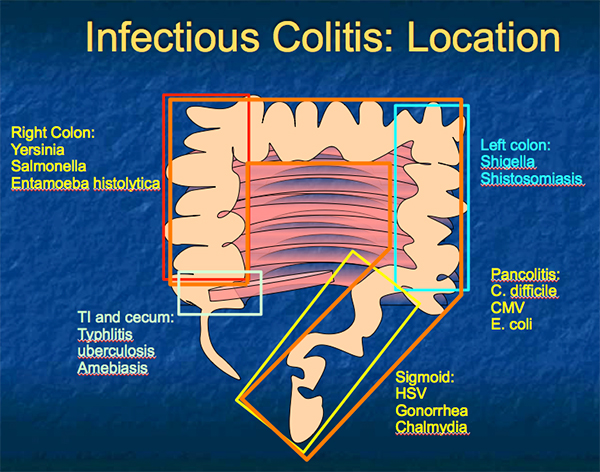
- Infectious Colitis: Location
- Pseudomembranous Colitis
• Clostridium difficile overgrowth
• Often due to antibiotic use
• Most commonly involves entire colon (pancolitis)
• may be limited to right colon in up to 40%
• CT signs:
• Significant wall thickening (can be > 3cm)
• Irregular or eccentric wall thickening
- Mural hypoattenuation (edema) or hyperattenuation (acute inflammation)
- Thumbprinting- thickened haustra
- “Accordion sign”- oral contrast between thickened haustra 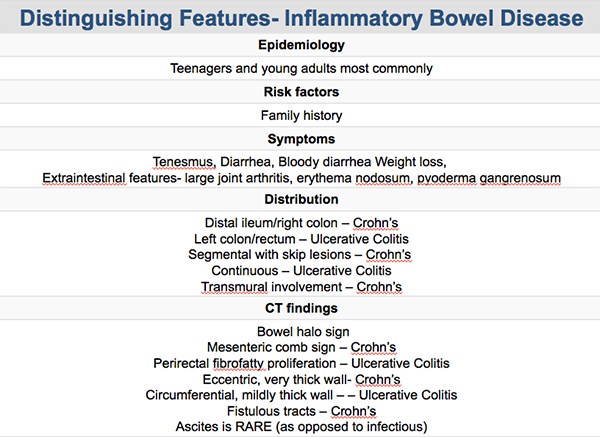
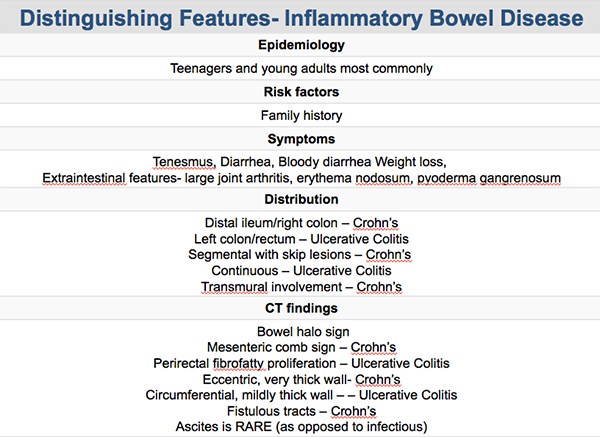
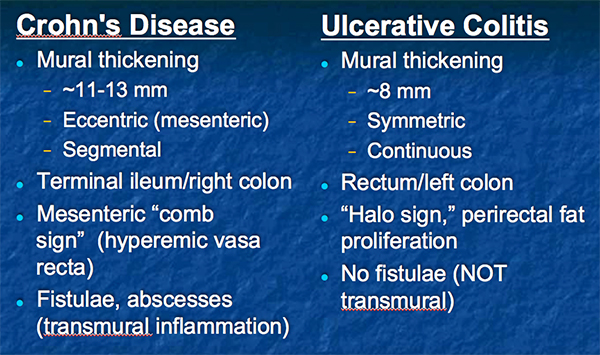
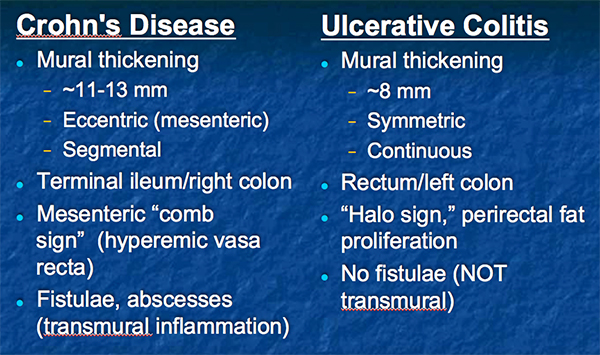
- CT of IBD: Crohn’s vs UC
- “ Inflammatory bowel disease (IBD) is a fairly common enteropathy that occurs in one per 1000 people in developed countries. The etiology of IBD is still unknown. The peak incidence of IBD is between the ages of 15 and 40 years, with a possible second peak between 50 and 80 years. Although controversial, several studies have reported a slight female predominance in Crohn disease and a male predominance in ulcerative colitis.”
Inflammatory Bowel Disease: Current Role of Imaging in Diagnosis and Detection of Complications Pedro Sergio Brito Panizza et al. RadioGraphics 2017; 37:701–702 - “The inflammatory mesentery group corresponds to three main findings: lymphadenopathy, fat changes, and engorged vasa recta. Reactive mesenteric lymphadenopathy can be characterized by nu- merous hyperenhancing small mesenteric lymph nodes. Fat changes represent fat stranding, which is a marker of active disease, and fibrofatty proliferation that is usually seen in patients with long-standing disease. Engorged vasa recta, also known as the “comb” sign, can be found surrounding the involved intestinal loop.”
Inflammatory Bowel Disease: Current Role of Imaging in Diagnosis and Detection of Complications Pedro Sergio Brito Panizza et al. RadioGraphics 2017; 37:701–702 - “The bowel wall disorders group represents three findings: wall thickening, strati cation, and permanent structural changes. Wall thickening is present in almost all patients with IBD, and evaluation of the thickening pattern and mural stratification provides important data to differentiate active from inactive disease. The “lead pipe” sign is the most important permanent structural change, represented by loss of haustrations in the colon, which is frequently related to ulcerative colitis.”
Inflammatory Bowel Disease: Current Role of Imaging in Diagnosis and Detection of Complications Pedro Sergio Brito Panizza et al. RadioGraphics 2017; 37:701–702 - “The disease complications group is striated into two subgroups: luminal complications (strictures, dilatations, and cancer) and extraluminal complications ( fistula, abscess, and perforation or toxic megacolon). Half of the patients with Crohn disease have intestinal complications within 20 years of disease onset. Strictures occur because of long-standing inflammation, may vary in length, and
are commonly associated with proximal bowel dilatation.”
Inflammatory Bowel Disease: Current Role of Imaging in Diagnosis and Detection of Complications Pedro Sergio Brito Panizza et al. RadioGraphics 2017; 37:701–702 - “Colorectal cancer has a much higher inci- dence in patients with IBD, and it occurs most often in the rectosigmoid, being that lymphoma
is more prevalent when there is involvement of the small bowel. Other important related cancers are cholangiocarcinoma and melanoma. Perforation and toxic megacolon represent the two main conditions that require emergency surgery.”
Inflammatory Bowel Disease: Current Role of Imaging in Diagnosis and Detection of Complications Pedro Sergio Brito Panizza et al. RadioGraphics 2017; 37:701–702
- “Acute colitis with megacolon occurs in approximately 10% of patients with ulcerative colitis and 2.3% with Crohn colitis. The definition of a megacolon varies between 5.5 and 8 cm depending on the author and the location of segment along the course of the colon. Most clinicians consider a colonic lumen greater than 6 cm to be a megacolon when colitis is present.”
Acute Infectious and Inflammatory Enterocolitides Baker ME Radiol Clin N Am 53 (2015) 1255–1271 - “The findings of a severe colitis on plain films and cross-sectional imaging (usually CT) include nodular or asymmetric fold thickening, submucosal edema, effacement of the fold pattern with thinning of the colonic wall, pericolonic soft tissue changes and/or edema, and uncommonly free intraperitoneal gas.”
Acute Infectious and Inflammatory Enterocolitides Baker ME Radiol Clin N Am 53 (2015) 1255–1271 - “When there has been thrombosis of a major vein, such as the superior mesenteric vein, cross- sectional imaging generally shows a long segment of symmetric small bowel wall thickening with mucosal hyperenhancement and submucosal low attenuation caused by edema. There is often adjacent mesenteric fat edema as well as ascites. If intravenous contrast has been injected, thrombus in the vein will be identified. Depending on the de- gree of ischemia and infarction, there may be pneumatosis and/or portal venous gas.”
Acute Infectious and Inflammatory Enterocolitides Baker ME Radiol Clin N Am 53 (2015) 1255–1271 - “In general, infections can affect both the small and large bowel. In the colon, most infections can cause a pancolitis. Right-sided disease tends to occur in Campylobacter, Salmonella, Yersinia, tuberculosis, and amebiasis. Left-sided disease tends to occur in schistosomiasis, shigellosis, herpes, gonorrhea, syphilis, and lymphogranuloma venereum. Cytomegalovirus (CMV) and Escherichia coli tend to be diffuse.”
Acute Infectious and Inflammatory Enterocolitides Baker ME Radiol Clin N Am 53 (2015) 1255–1271 - “Neutropenic colitis is an inflammatory process affecting the right colon, especially the cecum and terminal ileum in neutropenic patients. The neutropenia in most cases results from chemotherapy, commonly high-dose chemo- therapy used for patients after bone marrow transplant. When acutely ill with a fever and abdominal tenderness, these patients are commonly evaluated with CT.”
Acute Infectious and Inflammatory Enterocolitides Baker ME Radiol Clin N Am 53 (2015) 1255–1271 - “On CT, the cecum and/or right colon is thick walled and may have pneumatosis. There is pericolonic soft tissue stranding and often pericolic gutter fluid. It is often impos- sible to determine whether these findings are caused by neutropenic colitis or pseudomembranous colitis because these patients are both neutropenic and C difficile positive. Even so, patients are managed conservatively unless they show signs of toxicity.”
Acute Infectious and Inflammatory Enterocolitides Baker ME Radiol Clin N Am 53 (2015) 1255–1271
- “Clinical guidelines often recommend imaging of the abdomen with CT for the acute presentation of LUQ pain, given the relatively broad differential diagnosis for left upper quadrant abdominal pain, some of which are potentially life- threatening. While renal and adrenal causes of abdominal pain more classically localize to the flanks, acute disease in these organs results in referred pain to the upper quadrants often enough to merit inclusion in the differential diagnosis.”
Computerized tomography of the acute left upper quadrant pain Tirkes T et al. Emerg Radiol DOI 10.1007/s10140-016-1410-5 - “The results of this investigation revealed sensitivity for the CT abdomen and pelvis to be 69 %, which is moderately good in the setting of acute left upper quadrant pain. However, specificity was 100 %, indicating that if a specific diagnosis is made on CT examination, it is highly likely to represent the underlying pathology of the left upper quadrant pain.”
Computerized tomography of the acute left upper quadrant pain Tirkes T et al. Emerg Radiol DOI 10.1007/s10140-016-1410-5 - “Abdominal CT had 100 % specificity and 69 % sensitivity for finding the etiology of acute left upper quadrant pain. The underlying etiologies of left upper quadrant pain are quite variable. The most common etiologies that were correctly diagnosed with CT included renal stones, pancreatitis, diverticulitis, hernia, pneumonia, and rib fractures. The most common etiologies that were not detected on CT were gastritis, pancreatitis, urinary tract infection, and esophagitis.”
Computerized tomography of the acute left upper quadrant pain Tirkes T et al. Emerg Radiol DOI 10.1007/s10140-016-1410-5
- Toxic Megacolon: Facts
- Acute transmural fulminant colitis with neuromuscular degeneration and colonic dilatation
- Dilated ahaustral colon with pseudopolyps and air-fluid levels
- No specific diameter although often markedly dilated
- Patients are sick - Ulcerative Colitis: Federle Facts
- Chronic, idiopathic diffuse inflammatory disease
- Primarily involves colorectal mucosa and submucosa
- Diagnostic clue: pancolitis with decreased haustration and multiple ulcerations
- Location:
- Rectum (30%)
- Rectum + colon (40%)
- Pancolitis (30%) - Large Bowel Infections: Facts
- Number of different possible etiologies including pseudomembranous colitis, bacterial organisms (campylobacter, shigella, salmonella, E. coli, etc.) and parasites (E. histolytica)
- Clostridium difficile is by far the most common in daily practice
- Often arises in the setting of prior antibiotic therapy or chemotherapy
- Can be a fulminant colitis with high morbidity and mortality, and not uncommonly presents with GI bleeding
- Pancolitis with extensive pericolonic fat stranding, free fluid, and inflammatory change.
- Isolated involvement of right or transverse in up to 5% of cases - Aorto-Enteric Fistulae: Facts
- Life-threatening disorder with mortality of virtually 100%
- Primary or secondary forms
- Secondary most common – prior aortic surgery or raft placement
- Classic triad: Abdominal pain, massive GI hemorrhage, and pulsatile abdominal mass
- CT is the best initial modality:
- Ectopic gas within aortic lumen or adjacent to aorta
- Direct contrast extravasation from aorta to bowel or vice-versa is rare
- Effacement of fat plane between the aorta and adjacent bowel
- Focal bowel wall thickening adjacent to the aorta
- Periaortic soft tissue thickening and fluid, - Stercoral Colitis: Facts
- Primarily seen in elderly patients
- Overdistension of rectal lumen from impacted stool
- Increased luminal pressure results in rectal wall ischemia (disrupts blood supply)
- Ulcers of rectal wall result in bleeding and perforation
- Affects up to 6% of elderly patients in long-term care
- Active extravasation almost never visualized
- Slow, intermittent bleeding
- MDCT shows distended rectum with wall thickening and perirectal stranding
- Small and Large Bowel Infections
- Common cause of diarrheal illness in the US
- Vast majority are not imaged with CT
- Can be viral (norovirus, rotavirus), bacterial (Salmonella, E. coli, Clostridium perfringens, C. Dificile), or protozoal (cryptosporidum, microsporidum, etc.)
- Probably most common cause of bowel wall thickening in day-to-day practice
- Severe infections with any organism can cause lower GI bleeding; certain organisms more likely - Large Bowel Infections
- Number of different possible etiologies including pseudomembranous colitis, bacterial organisms (campylobacter, shigella, salmonella, E. coli, etc.) and parasites (E. histolytica)
- Clostridium difficile is by far the most common in daily practice
- Often arises in the setting of prior antibiotic therapy or chemotherapy
- Can be a fulminant colitis with high morbidity and mortality, and not uncommonly presents with GI bleeding
- Pancolitis with extensive pericolonic fat stranding, free fluid, and inflammatory change.
- Isolated involvement of right or transverse in up to 5% of cases - Aortoenteric Fistula
- Life-threatening disorder with mortality of virtually 100%
- Primary or secondary forms
- Secondary most common – prior aortic surgery or graft placement
- Classic triad: Abdominal pain, massive GI hemorrhage, and pulsatile abdominal mass
- CT is the best initial modality:
- Ectopic gas within aortic lumen or adjacent to aorta
- Direct contrast extravasation from aorta to bowel or vice-versa is rare
- Effacement of fat plane between the aorta and adjacent bowel
- Focal bowel wall thickening adjacent to the aorta
- Periaortic soft tissue thickening and fluid
- GI Tract Complications: Chemotherapy
- Stomach- ulcers and gastritis
- Small bowel-enteritis with changes including ulceration, target sign, strictures
- Large bowel-pneumatosis (benign or malignant), necrosis, ischemia, neutropenic colitis, pseudomembranous colitis, perforation, typhlitis
- Complications of oncologic therapy in the abdomen and pelvis: a review
Ganeshan DM et al.
Abdom Imaging (2013) 36:1-21 - Typhlitis: Facts
- Triad includes fever, abdominal pain, and neutropenia
- Distension and diffuse circumferential thickening of the cecal wall
- Stranding in pericolonic fat around cecum
- Pneumatosis, perforation or pneumoperitoneum may also occur - GI Tract Complications: Radiation Therapy
- Stomach- ulcers and gastritis
- Small bowel- radiation enteritis which usually resolves 2-6 weeks post therapy
- Large bowel- radiation colitis
- Liver- fatty infiltration in geographic pattern
- Complications of oncologic therapy in the abdomen and pelvis: a review
Ganeshan DM et al.
Abdom Imaging (2013) 36:1-21
- Infectious Enterocolitis : Key Facts
- May be caused by agents including Yersinia, Campylobacter or Salmonella
- CT shows terminal ileum thickening without inflammatory mass but often with nodes - Crohns Disease : Key Facts
- Patients with crohns may initial present as suspected appendicitis
- Key is symmetric wall thickening and fibrofatty proliferation - "Our results suggest that CT findings of colonic wall thickening in end stage liver disease should be considered benign, and colonoscopy is unnecessary for the evaluation of malignancy or colitis unless it is clinically indicated."
Colonoscopy Findings in End Stage Liver Disease Patients with Incidental CT Colonic Wall Thickening
Ormsby EL et al.
AJR 2007; 189:1112-1117 - "The colonoscopy changes primarily ranged from mild mucosal edema to increased vascularity and telangiectasia, probably from hypoproteinemia or portal hypertension."
Colonoscopy Findings in End Stage Liver Disease Patients with Incidental CT Colonic Wall Thickening
Ormsby EL et al.
AJR 2007; 189:1112-1117